What are the Top 9 Most Common Food Allergies and How Pharma Companies are Tackling the Crisis?
Mar 23, 2022
Table of Contents
Food Allergies is a major concern for a wide spectrum of populations globally. According to the World Allergy Organization, “food allergy affected approximately 2.5% of the general population, but the spread of prevalence data was wide, ranging from 1% to 10%.” According to the Centers for Disease Control and Prevention, the rising prevalence of food allergies is growing food safety and public health concerns, it is estimated 8% of children in the US are affected by different food allergies.
As per DelveInsight Food Allergy Epidemiology Analysis, the total Food Allergy prevalent cases in the 7MM, Canada and China were more than 285 million in 2021, which is expected to increase in the coming years.
Downloads
Article in PDF
Recent Articles
- Notizia
- Allergy Diagnostics: Unraveling the Science, Market Trends, and Future Prospects
- Neurotech’s ENCELTO Becomes First FDA-Approved Treatment for MacTel Type 2; Plus Therapeutics’ Rh...
- Egg Allergy Market: Second most common food allergy but no approved therapy
- Revolutionizing the Food Allergy Treatment: The Impact of Xolair’s Approval
The prevalence has risen significantly over the past few years and the trends vary widely across age groups, different geographical locations and are also closely related to the cultures on dietary habits. For better understanding, we can take a look at the peanut allergy prevalence, it is quite high in the US and UK, while relatively low in Italy and Spain. Similarly, in the middle east, the Sesame allergy is most prevalent as compared to other geographical locations and it is the third most common food allergen in Israel.
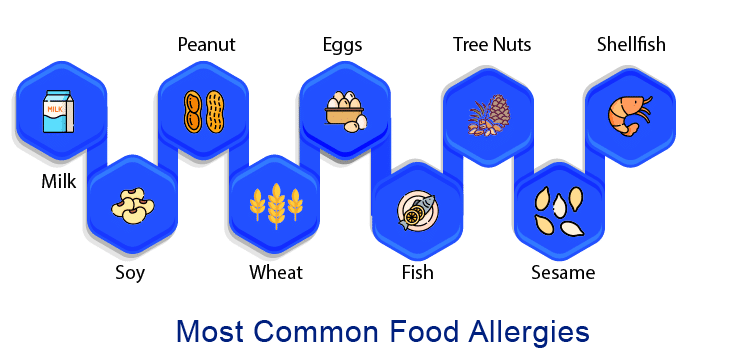
Due to variation in Food Allergies prevalence, different countries globally have created a food allergies list that comprises the most common allergies. In the United States, under the Food Allergen Labeling and Consumer Protection Act of 2004 (FALCPA), the food allergies list contains milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soybeans, as the most common Food Allergen.
What is a Food Allergy? What are its Most Common Symptoms?
“Allergy” and “allergic disease” are terms used to describe conditions that involve immune system changes. These immune system changes are classified as IgE-mediated or non-IgE-mediated. But the most common question that arises to everyone is, are food allergies genetic? So the answer is Food allergies can be inherited, but this does not imply that an allergy to a specific food is inherited or that everyone with a food allergy inherits it from their parents.
Food Allergy causes can be functional genetic variants in the IL-12 receptor b1, Toll-like receptor 9, and thymic stromal lymphopoietin genes, and even IL-4 gene polymorphism has been linked to an increased risk of food sensitization.
Food Allergy symptoms may be triggered in the skin (itching, redness, swelling), gastrointestinal tract (pain, vomiting, diarrhoea, itching and swelling of the oral cavity), respiratory tract (itching and swelling of the nose and throat, asthma), eyes (itching and swelling), and cardiovascular system (chest pain, abnormal heart rhythm). In addition, severe life-threatening Food Allergy reactions require immediate medical attention.
There are several misconceptions regarding food allergy and food intolerance. Both the terms are commonly confused by a large segment of the population. Food allergy is an immune system reaction and often happens quickly. The Food Allergy can be triggered by even a minute amount of the food. On the other hand, food intolerances are an adverse reaction to food and may take hours to days to manifest. Food intolerances are not associated with the immune system of the body. Additionally, it is a must to note that, Food Allergy and Food Intolerance have several overlapping symptoms.
Food Allergy diagnosis is based on the patient’s history and physical exam. According to the World Allergy Organization (WAO), the most common Food Allergy diagnosis methods are Skin Prick Tests (SPT), which is the preferred Food Allergy testing method in patients; double-blind placebo-controlled food challenge (DBPCFC), which is the preferred test for Food Allergy diagnosis; In vitro diagnostics can aid in the identification of cross-reactive allergens between pollen and foods, or foods and latex, and the Atopy Patch Test (APT) is an epicutaneous skin test that uses allergens commonly associated with IgE reactions.
Some of the Most Common Food Allergies –
Milk (Cow Milk)
Cow’s milk allergies are the most common allergies in babies and young children, especially if they have been exposed to cow’s milk protein before the age of six months. It’s one of the most common childhood food allergies, affecting 2–3% of infants and toddlers. However, 90% of children outgrow the condition by the age of three, making it much less common in adults. As per DelveInsight, the total Cow Milk Allergy prevalent cases in the 7MM were approximately 10.7 million in 2021.
Cow’s milk allergies can be IgE or non-IgE, but IgE cow milk allergies are the most common and potentially the most severe. Children and adults with IgE allergies usually have a reaction within 5–30 minutes of consuming cow’s milk. The typical sign of milk allergy includes swelling, rashes, hives, coughing, stomach upset, vomiting, and, in rare cases, anaphylaxis. A non-IgE milk allergy can be difficult to identify. This is due to the fact that symptoms can sometimes indicate an intolerance, and there is no blood test for it. If a cow’s milk allergy is diagnosed, the only treatment is to avoid cow’s milk and foods containing it. This includes any foods or beverages containing the following ingredients: milk, milk powder, cheese, butter, margarine, yoghurt, cream, or ice cream.
Breastfeeding mothers of allergic babies may have to eliminate cow’s milk and foods containing it from their own diets. A suitable alternative to a cow’s milk-based formula will be recommended by a health professional for babies who are not breastfeeding. Currently, Nestle, Danone, and Reckitt Benckiser are controlling the majority of the lactose intolerance market. Along with these three, the other major companies include Abbott, FrieslandCampina, Bellamy’s Organic, Kraft Heinz, HiPP GmbH & Co., Vertrieb KG, Perrigo, and Arla Foods.
Peanut Allergy
Peanut Allergy is a condition in which the immune system of the body does not recognise peanut protein and misidentifies even trace amounts of peanut as harmful. Allergic reactions to peanuts are unpredictable in their occurrence and presentation, with some people experiencing severe reactions to even trace amounts. Peanut allergy symptoms can range from mild to severe anaphylactic reactions such as urticaria – a red, blotchy, and intensely itchy skin rash commonly known as hives. Swelling (angioedema) of the face, eyelids, lips, tongue, the roof of the mouth, or throat is also a symptom, as are abdominal cramps, diarrhoea, nausea, vomiting, and a runny and itchy nose. But the most common reaction in Peanut Allergy patients is anaphylaxis. Peanut Allergy is diagnosed by examining a patient’s diet history as well as the severity and duration of their symptoms after being exposed to peanuts. Following that, a skin test for allergy or a blood sample to check for IgE may be performed. A positive challenge test, in which the peanut protein is administered to the patient to examine their allergic reaction, may be performed in rare cases.
Peanut Allergy prevalence has steadily increased over the last few decades. As per DelveInsight, the total Peanut Allergy prevalent cases in the 7MM were more than 6.6 million in 2021.
In 2020, the FDA has approved Aimmune Therapeutics’ Palforzia to treat allergic reactions, including anaphylaxis, caused by accidental peanut exposure. Palforzia is the first FDA-approved treatment for patients with Peanut Allergies. It is made up of carefully selected doses of peanut powder that are taken orally. It is intended for children and teenagers aged 4–17 who are allergic to peanuts. The goal is to desensitise kids to peanuts.
Moreover, the recent increase in funding has resulted in new products in the pipeline, as well as persistently rising cases of peanut allergies, which will help proliferate the Peanut Allergy treatment market. The major pharmaceutical companies such as Nestle Health Sciences, DBV Technologies, Regeneron, Sanofi, Camallergy, Vedanta Biosciences, Alladapt Immunotherapeutics, InnoUp Farma, COUR Pharmaceuticals, Novartis, Genentech, and others working in the Peanut Allergy market to improve the treatment landscape. Furthermore, as per DelveInsight estimates, the Peanut Allergy market size was USD 360.8 million in 2020, which is further expected to increase by 2030.
Browse through our blogs to learn more about the Peanut Allergy Treatment Market Landscape
Wheat
Wheat allergy is one of the most common allergies in children and adults. The Wheat allergy signs and symptoms start appearing after a few minutes to hours of eating something containing wheat or in some cases it may be due to inhaling wheat flour. Gluten is a protein found in some grains such as barley, rye and wheat. It is observed that Some people may be allergic to wheat but that is not the same as a gluten allergy. In some cases, wheat allergy is often confused with wheat allergy or celiac disease.
As per DelveInsight’s assessment, the total Wheat Allergy prevalent cases in the 7MM were around 4.2 million in 2021.
The common Wheat Allergy Triggers may include bread, pasta or wheat-based ingredients, such as Play-Doh, cosmetics or bath products. Some of the most common Wheat allergy symptoms include headache, sneezing, swelling, asthma, hives or rash, itching, or irritation in the mouth and throat, trouble in breathing, cramps, nausea, vomiting, diarrhoea, among several others. In some rare cases, the wheat allergy may cause a life-threatening reaction called anaphylaxis.
Upon diagnosis with Wheat allergy, the patients are more likely to recommend Antihistamines or an epinephrine auto-injector. Antihistamines can help to overcome signs and symptoms for some minor wheat allergies. Similarly, epinephrine is administered as an emergency treatment for anaphylaxis.
Eggs
After the Cow Milk allergy, egg allergy is the second most common food allergy in children. Egg allergy occurs when the body’s immune system becomes sensitized or overreacts to proteins in the egg. Alpha-livetin (Gal d 5) present in the egg yolk is one of the major allergens. Some of the most common egg allergy symptoms include skin rashes, throat tightness, hives, nasal congestion, hoarseness, vomiting, belly pain, swelling, or other digestive problems.
According to one of the studies by Salo et al., in the US, “prevalence estimates for sensitization was 3.4% to the egg in the overall population aged 6 and above.” In the UK, it is estimated that one in 20 develops egg allergy in the United Kingdom (as per the data by Allergy UK). Similarly, As per DelveInsight, the total Egg Allergy prevalent cases in the 7MM were over 5 million in 2021.
Currently, there are no approved therapies for the treatment of egg allergy. Avoidance is the best management for eggs allergy. However, eggs are one of the major ingredients in many foods. The avoidance may lead to dietary limitations and one’s quality of life. To overcome the Eggs allergy physician may prescribe Antihistamines to relieve mild symptoms of egg allergy, such as itching. Epinephrine (adrenaline) may be prescribed in an auto-injector form, for all patients with a history of anaphylactic reactions to an egg and typically for patients with milder IgE-mediated reactions to an egg as well. Globally, some of the key pharma and biotech companies such as Genentech, Novartis, Aimmune Therapeutics, DBV Technologies, Alletess Medical Laboratory, Kaleo, Inc., Mylan NV, Sanofi SA, ImmuneTech, HYCOR Biomedical, and others, are actively working to develop new treatment therapies for Egg Allergy. Several of the Eggs Allergies therapies are in the advanced stage of clinical development, expected to hit the market in the near future.
Fish
As per DelveInsight, the total Fish Allergy prevalent cases in the 7MM were approximately 6.1 million in 2021. Fish allergy has a prevalence of 1% in the US. Some people are allergic to only some of the fish. One of the studies on Fish allergy suggested that salmon, tuna, catfish and cod are some of the fish to which people most commonly found to have allergic reactions.
Commonly the Fish symptoms develop when someone consumes fish, however, in some cases, the reactions may develop when the person touches the fish or breathes in vapours from cooking fish. It is worth noting that a fish allergy is not exactly the same as a seafood allergy. Seafood includes fish (like tuna or cod) and shellfish (like lobster or clams). Like other allergens, the Fish allergy may lead to symptoms such as coughing, wheezing, hoarseness, throat tightness, diarrhoea, itchy, watery, or swollen eyes, hives, among several others. Some of the fish may cause immediate, severe, and life-threatening complications. Majorly, fish allergy is treated with epinephrine (adrenaline) to reduce the symptoms of a reaction. In some cases when the patient develops Anaphylaxis, it can be fatal. To avoid Anaphylaxis, only epinephrine is recommended.
Tree Nuts
Tree nuts are common in both children and adults. Tree nuts include walnut, almond, hazelnut, pecan, cashew and pistachio. Tree nuts are different from peanuts, which grow underground and are considered legumes.
As per DelveInsight, the total Tree nuts Allergy prevalent cases in the 7MM were more than 7.2 million in 2021. As per the American Academy of Allergy, Asthma & Immunology (AAAAI), “Tree nut allergy is one of the eight most common food allergies, affecting roughly 0.5 to 1% of the U.S. population.” Tree nuts allergy is started during childhood and may remain lifelong. However, in nearly 10% of cases, the affected person may outgrow tree nut allergy with time. The basic mechanism for the Tree nuts allergy is that when the person consumes a tree nut, the proteins in the nut bind to specific IgE antibodies made by the person’s immune system. The binding triggers immune defences that may lead to some allergic symptoms, which can be fatal in some cases. Some of the Tree nuts allergy symptoms can occur promptly. Antihistamines and auto-injector (such as an EpiPen) to treat anaphylaxis immediately, are generally advised to the Tree nuts allergy affected person.
Sesame
In the United States, nearly 1.5 million people including both children and adults are allergic to Sesame. It is most common in children, but it can develop at any age. Only about 20-30% of childhood with sesame allergies eventually outgrow with time.
A sesame allergy can be developed due to coming in contact with the sesame plant, sesame products (like sesame seeds or sesame oil). The Sesame is not that much-hyped as compared to other allergens. However, it can be very fatal in some cases with life-threatening conditions such as anaphylaxis. Sesame allergy is found to be more common among children who already have other food allergies. Some of the common symptoms of Sesame allergy include a flushed face, hives or a rash, red and itchy skin. Swelling of the eyes, face, lips, throat and tongue. Trouble breathing, speaking or swallowing.
Only a few food companies clearly labelled sesame ingredients on their product labels, which makes it difficult for people with sesame allergies to buy and access the safety information. On April 23, 2021, FASTER Act was passed into law, according to which sesame be labelled on all packaged foods in the United States starting on Jan. 1, 2023. Over the past few years, the number of people who have reported Sesame allergy has risen significantly. Antihistamines and epinephrine are the first-line treatment for Sesame allergy.
Soy Allergy
Soy allergies affect approximately 0.4% of children and are most common in infants and children under the age of three. They are triggered by a protein found in soybeans or products containing soybeans. However, approximately 70% of children who are allergic to soy outgrow their allergies. As per DelveInsight, the total Soy Allergy prevalent cases in the 7MM were more than 2.3 million in 2021.
The symptoms can range from an itchy, tingly mouth and runny nose to a rash and asthma or breathing problems. Soy allergies can cause anaphylaxis in rare cases. Surprisingly, some babies who are allergic to cow’s milk are also allergic to soy. Soybeans and soy products such as soy milk or soy sauce are common soy allergy triggers. Because soy is present in so many foods, it is critical to read food labels. Soy allergy risk factors include family history, existing food allergies, and age. The first step in preventing soy allergy is to avoid soy and soy products. Moreover, Antihistamines may help to alleviate the signs and symptoms of minor Soy allergies. Taking an antihistamine after being exposed to soy may help control your reaction and alleviate discomfort.
Shellfish Allergy
A Shellfish allergy is caused when the body is attacked by the proteins found in the crustacean and mollusc families of fish, which are commonly referred to as shellfish. Shellfish include shrimp, prawns, crayfish, lobster, squid, and scallops. According to DelveInsight, the total Shellfish Allergy prevalent cases in the 7MM were over 8.8 million in 2021. As per estimates, approximately 2% of the US population has an allergy to shellfish and it is observed that the Shellfish allergies are usually lifelong. Tropomyosin, a protein, is the most common cause of a seafood allergy. Arginine kinase and myosin light chain are two other proteins that may be involved in the initiation of an immune response. Allergic reactions can cause mild symptoms such as itching, hives, and eczema, but they can also lead to a potentially fatal condition known as anaphylaxis. Shellfish allergy can occur at any age, but it is more common in adults than in children.
Shellfish allergies typically manifest quickly and are similar to other IgE food allergies. On the other hand, a true seafood allergy can be difficult to distinguish from an adverse reaction to a contaminant of seafood, such as bacteria, viruses, or parasites. This is due to the fact that the symptoms are similar, as both can cause digestive issues such as vomiting, diarrhoea, and stomach pain. Because shellfish allergies do not usually resolve with time, most people with the condition must avoid all shellfish in their diet to avoid an allergic reaction. Surprisingly, the vapours from cooking shellfish can cause a shellfish allergy in those who are allergic. As a result, many people are advised to avoid being near seafood while it is being cooked.
Therapeutic Developments in the Food Allergies Market
Currently, the avoidance of the concerned food items is the only proven medication for food allergy. However, it is not always possible to avoid food items all the time from the diet. Therapies like antihistamines, injectable epinephrine, and immunotherapies are available in the market but they are only recommended to eliminate the symptoms. In severe anaphylaxis, ventilatory and circulatory support may be needed. Globally, some of the key companies are actively working in the development of new therapies for the treatment of various food allergies.
Currently, some of the major pharma and biotech giants with their therapies in various stages of development include Palforzia (Aimmune), Viaskin (DBV Technology), Ligelizumab (Novartis Pharmaceuticals), CNP-201 (COUR Pharmaceutical Development Company, Inc.), INP20 (InnoUp Farma S.L.), ADP101 (Alladapt Immunotherapeutics, Inc.), and others.
Recent Developments in the Food Allergies Treatment Market
Over the past few years, there have been several clinical and commercial developments in the Food Allergies Treatment Market. Some of the major developments in the Food Allergy market landscape include –
- In January 2020, FDA approved Aimmune Therapeutics’s Palforzia (AR101) for the treatment of food allergies. It is the first approved treatment for patients with Food Allergies.
- In 2021, Cour Pharmaceuticals announced that the US FDA has accepted the company’s Investigational New Drug (IND) application for evaluation of COUR’s CNP-201 in a proof-of-concept (Phase I / II) study in people who are allergic to peanuts.
- On March 2022, Aravax Pty Ltd announces the opening of IND for Phase 2 clinical trials of PVX108, next-generation immunotherapy for the treatment of peanut allergy.
Learn more about the latest developments in the Food Allergies Market in our latest healthcare report, at Food Allergy Market Forecast – 2032
Food Allergies Treatment Market Outlook
As the global prevalence of food allergy is growing exponentially, the demand for new and effective therapies is also rising significantly. As per DelveInsight’s assessment, the Food Allergy market size was found to be USD 2,028.97 Million in 2021 in the 7MM (i.e the US, the UK, Japan, Spain, France, Italy, Germany), Canada, and China. The therapeutics market is expected to grow in the coming years. Among the 7MM, the US accounted for 53% Food Allergy Market Share of the overall market size. Similarly, Spain accounts for the highest market size for Food Allergy among the EU5 countries.
The Food Allergy Therapeutics Market will evolve immensely in the near future owing to the active participation of the key companies and the launch of the emerging therapies such as Omalizumab as Monotherapy and as Adjunct Therapy to Multi-Allergen OIT, Ligelizumab, CA002, VE416, and others.

Frequently Asked Questions (FAQ)
“Allergy” and “allergic disease” are terms used to describe conditions that involve immune system changes. These immune system changes are classified as IgE-mediated or non-IgE-mediated.
Food Allergy symptoms may be triggered in the skin (itching, redness, swelling), gastrointestinal tract (pain, vomiting, diarrhoea, itching and swelling of the oral cavity), respiratory tract (itching and swelling of the nose and throat, asthma), eyes (itching and swelling), and cardiovascular system (chest pain, abnormal heart rhythm).
Currently, the avoidance of the concerned food items is the only proven method to overcome food allergies. However, it is not always possible to avoid food items all the time from the diet. Additionally, antihistamines, injectable epinephrine, and immunotherapies are available in the market that can help to reduce the symptoms.
The leading players working in the Food Allergy market include Aimmune Therapeutics, Inc., Novartis Pharmaceuticals, DBV Technologies, InnoUp Farma S.L., COUR Pharmaceutical Development Company Inc., Vedanta Biosciences, Inc., Regeneron Pharmaceuticals, Genentech, Inc., Rho Federal Systems Division, Inc., Alladapt Immunotherapeutics, Inc., Camallergy, Abbott, FrieslandCampina, Bellamy’s Organic, Kraft Heinz, HiPP GmbH & Co., Vertrieb KG, Perrigo, Arla Foods, Sanofi, among others.
The emerging Food Allergies therapies include Palforzia, Ligelizumab, Viaskin Peanut, INP20, CNP-201, VE416, Dupilumab, Omalizumab, ADP101, CA002, and others.
Downloads
Article in PDF
Recent Articles
- Zydus starts Phase II COVID-19 vaccine trial; Taysha raises $95M; FDA declines DBV’s peanut...
- Allergy Diagnostics: Unraveling the Science, Market Trends, and Future Prospects
- Notizia
- Dupixent Significantly Reduced COPD Exacerbations; Sosei Heptares to Regain Ownership of GSK43814...
- Egg Allergy Market: Second most common food allergy but no approved therapy