Rising Acute Respiratory Distress Syndrome (ARDS) Prevalence Posing a Major Public Health Concern
Nov 20, 2024
The acute respiratory distress syndrome (ARDS) prevalence is increasing every year; it is estimated that in the United States alone, about 190K Americans are diagnosed with ARDS each year. Prior to the COVID-19 global pandemic, more than 700K individuals in the US and 2 million cases globally developed ARDS from trauma, sepsis, bacterial, and viral infections, with a cumulative mortality of 40%. The COVID-19 pandemic has highlighted several severe unmet needs in the ARDS domain these include starting with the lack of effective FDA-approved pharmacotherapies, as neither SARS-CoV-2 vaccinations nor anti-SARS-CoV-2 vaccines address the unregulated inflammation that promotes multiorgan failure and ARDS death.
Despite recent advances in translational research and exponential growth in the identification of new biomarkers, precision medicine approaches to ARDS have yet to be deployed, and validated ARDS biomarkers are lacking. This critical unmet need in ARDS emphasizes a crucial gap between the rapid rate of biomarker discovery and effective translation to clinical application, as well as the need for biomarkers to influence a more streamlined drug approval process. The absence of accurate and validated ARDS biomarkers is one of the many reasons why clinical studies in ARDS fail.
Acute Respiratory Distress Syndrome Epidemiology Insights
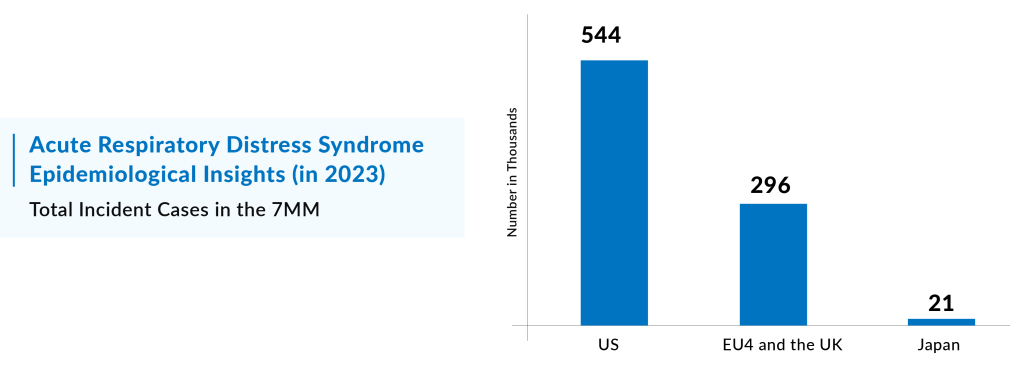
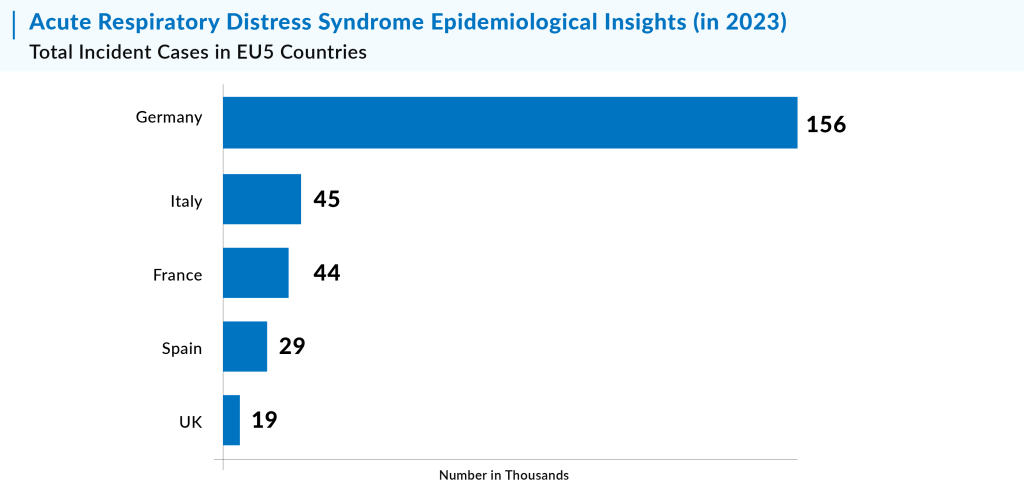
In 2023, the total incident cases of Acute Respiratory Distress Syndromein the United States were approximately 591 thousand. The United States accounted for the largest share of the ARDS population, representing about 62% of the total cases across the 7MM (United States, EU4, UK, and Japan). Meanwhile, the EU4 countries (Germany, France, Italy, and Spain) and the UK, along with Japan, contributed approximately 34% and 4% of the total Acute Respiratory Distress Syndrome market share in 2023, respectively.
Downloads
Article in PDF
Recent Articles
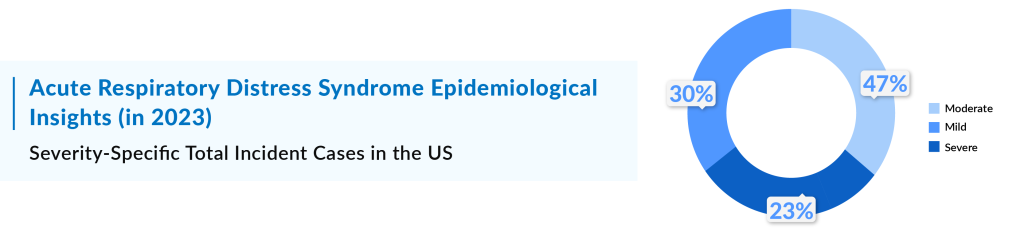
In 2023, there were 177,000 cases of acute respiratory distress syndrome (ARDS) in the U.S. classified as mild severity. This distribution highlights the varying treatment approaches required, ranging from less intensive care for mild cases to more aggressive interventions for severe cases.
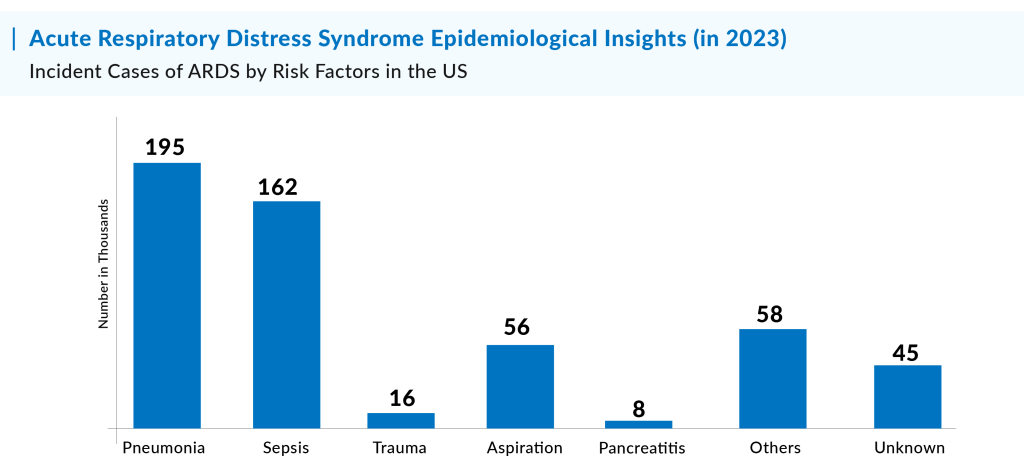
DelveInsight estimates indicate that 210,000 incident cases of ARDS in the U.S. in 2023 were primarily caused by pneumonia, followed by sepsis, aspiration, and other contributing factors. Additionally, cases with unknown origins also made up a significant portion of the total.
Driving Factors and Epidemiological Trends for ARDS Prevalence
Pneumonia, Sepsis, Aspiration, Trauma, Pancreatitis, and others are among the major driving factors for ARDS prevalence. With the increase in the cases of these factors, the prevalence of ARDS is expected to rise in the coming years. As a result, the future trend of ARDS epidemiology is anticipated to be the same, but pneumonia and sepsis are expected to be key factors for the surge in the ARDS prevalence by 2034.
Other the other hand, acute respiratory failure-related mortality has increased at a rate of around 3.4% per year, and there has been no drop in ARDS-related mortality in the previous five years. This concerning tendency is constant across age, gender, race and ethnicity, urbanization, and geographical regions. Identifying these tendencies and adjusting public health and policy planning efforts to them may assist to direct resource and infrastructure organization for the massive morbidity and death burden that is projected in the United States with the full-scale of ARF and ARDS linked with COVID-19.
Way ahead
Acute respiratory failure (ARF) is a critical condition that often sends patients straight to the ICU, where they face the harsh reality of mechanical ventilation. When ARF is caused by severe lung damage, it progresses into a life-threatening condition known as Acute Respiratory Distress Syndrome (ARDS). ARDS is an inflammatory disease that leads to fluid buildup in the lungs, making it difficult for oxygen to reach the bloodstream. It results in hypoxemia—low oxygen levels—and can leave patients struggling for breath, often with a poor prognosis. Historically, ARDS has been one of the leading causes of ARF, affecting nearly 3 million people every year. This disease is responsible for 10% of ICU admissions and 24% of mechanical ventilation cases, with a staggering mortality rate of 35-46%, depending on the severity of the disease when it strikes.
Once, the COVID-19 pandemic was a major driving force behind the surge in ARDS cases, with patients experiencing severe respiratory distress due to viral pneumonia. However, with the pandemic subsiding, pneumonia has now become the predominant cause of ARDS in many cases, alongside other pulmonary and nonpulmonary causes such as trauma, pancreatitis, and sepsis. Despite significant advances in understanding the pathogenesis, development, and therapy of ARDS and ARF, current statistics on the mortality burden of ARF and ARDS in the United States are inadequate. There remains a significant gap in comprehensive data, particularly after the adoption of the Berlin criteria for ARDS diagnosis. These gaps are concerning, especially given the role of geographic disparities in the quality of care. Different regions have varying access to critical care resources, which can heavily influence outcomes for ARDS patients.
The burden of ARDS is high, but the clinical landscape continues to evolve. Pneumonia has emerged as a significant contributor to ARDS, reshaping the way we approach treatment and management. Advances in research and clinical practices are slowly chipping away at the high mortality rates, but with ongoing infrastructural challenges, especially in the ICU, much work remains to be done. This evolving story of ARDS highlights the need for continuous improvements in healthcare systems, better data collection, and more focused attention on how regional differences impact care, ultimately striving for a world where ARDS no longer carries such a heavy toll.
Downloads
Article in PDF
Recent Articles
- Will there be a second wave of coronavirus?
- Merck, Gilead teams up for HIV treatment; Bright Future for Sanofi/Regeneron’s Libtayo; Roche acq...
- Algernon’s NP-120; FDA nod to 4DMedical tool; SaNOtize’s NORSTM trial; Pole’s c...
- Supply shortage: Why ventilators are in demand amid the Coronavirus crisis
- Ocugen-Bharat Biotech’s Covaxin Against B.1.617 Corona Variant; uniQure Shares; J&J Covid Va...