5 Promising Exosome-based Therapies Paving the Way for Personalized Medicine
Oct 25, 2024
Table of Contents
Exosome therapies represent an exciting frontier in the development of novel treatments for a wide range of diseases. The ability to harness the natural communication system of cells offers unparalleled potential for precise and effective treatments. While challenges remain, ongoing research and technological advancements are paving the way for exosome-based therapies to become a cornerstone of modern medicine.
Although exosome technology is still very much in its clinical infancy, it represents an innovative drug delivery platform that is starting to make its way into the clinic. At present, extracellular vesicles are being investigated for a range of potential therapeutic and diagnostic uses. As the field continues to evolve, we are likely to witness a new era of personalized, targeted therapies that could dramatically improve patient outcomes across multiple medical disciplines.
Downloads
Article in PDF
Recent Articles
- FDA Approves Jardiance for Type 2 Diabetes; FDA Approves Pfizer’s LITFULO for Alopecia Areata; Sa...
- Zealand Pharma’s Phase III Results of Glepaglutide; FDA Approves Amylyx’s ALS Drug Relyvrio; Novo...
- Nucleic Acids and Gene Therapies in Neuromuscular Disorders: Next-Generation Therapeutic Strategies
- Bristol-Myers Squibb’s Opdivo Approval; Mirati’s KRAS-inhibitor Adagrasib; J&J and Legend Bi...
- Aslan Pharma – IQVIA collaboration; Reata’s kidney drug bardoxolone; Alzheimer’s Dise...
5 Promising Exosome Therapies in the Pipeline
Exosomes are emerging as a promising frontier in therapeutics, with exosome-based treatments becoming an active area of research. These therapies have the potential to revolutionize fields such as drug delivery, regenerative medicine, and diagnostic approaches. The function of exosomes is entirely dependent on the source of the donor cells and can have both beneficial and harmful effects.
In regenerative medicine, particularly in the use of incubated cell preparations, exosomes show potential as disease-modifying therapies for autoimmune disorders. However, it is important to note that exosome therapies are not yet FDA-approved and should only be used within research protocols or submitted for FDA Biologics License Applications.
Exosome-based therapies are still emerging, but exosomes have demonstrated promise in supporting tissue repair and regeneration, and are under investigation for their potential application in treating various conditions, including autoimmune diseases, cardiovascular disorders, neurological conditions, as well as bone and cartilage injuries.
Some of the exosome drugs in the pipeline include CAP-1002 (Capricor Therapeutics), ExoFlo (Direct Biologics), AGLE-102 (Aegle Therapeutics), ILB-202 (ILIAS Biologics), and BRE-AD01 (Brexogen) among others. Let’s dive deep into the detailed assessment of these therapies.
Capricor Therapeutics’ CAP-1002
CAP-1002 (deramiocel) is composed of cardiosphere-derived cells, which are precursor cells that generate heart cells and produce small vesicles known as exosomes. These exosomes play a role in regulating immune system activity and promoting cellular regeneration. The drug is currently undergoing Phase III clinical trials for treating Duchenne muscular dystrophy.
In August 2024, Capricor Therapeutics announced a successful pre-BLA meeting with the FDA that took place in the third quarter of 2024. Furthermore, Capricor shared encouraging results from the 36-month follow-up of the HOPE-2 OLE study at the Parent Project Muscular Dystrophy (PPMD) Annual Conference. The Phase III HOPE-3 trial for deramiocel in DMD is fully enrolled and is expected to provide top-line results from Cohort A in the fourth quarter of 2024.
Direct Biologics’ ExoFlo
ExoFlo is an extracellular signal product derived from human bone marrow mesenchymal stem cells (MSCs) and is rich in growth factors and extracellular vesicles, including exosomes. Direct Biologics is currently running the global Phase III EXTINGUISH ARDS clinical trial to evaluate ExoFlo for treating hospitalized adults with moderate to severe ARDS. Furthermore, the company has begun Phase I clinical trials of ExoFlo for ulcerative colitis and Crohn’s disease, as well as expanded access trials for solid abdominal organ transplantation and severe ARDS patients.
Aegle Therapeutics’ AGLE-102
AGLE-102 comprises COL7 protein and COL7A1 mRNA, which has been shown in preclinical models to stimulate Recessive Dystrophic Epidermolysis Bullosa (RDEB) cells, which cannot produce COL7, to generate it. This therapy has the potential to promote functional regeneration and the organization of complex tissue structures in patients with dystrophic epidermolysis bullosa and epidermolysis bullosa, potentially speeding up healing, minimizing scarring, and enhancing overall appearance.
Furthermore, AGLE-102 is non-immunogenic and possesses the immunomodulatory and anti-inflammatory properties associated with mesenchymal stem cells (MSCs). Aegle’s Phase I/II clinical trial of AGLE-102 for individuals with RDEB is currently open for enrollment.
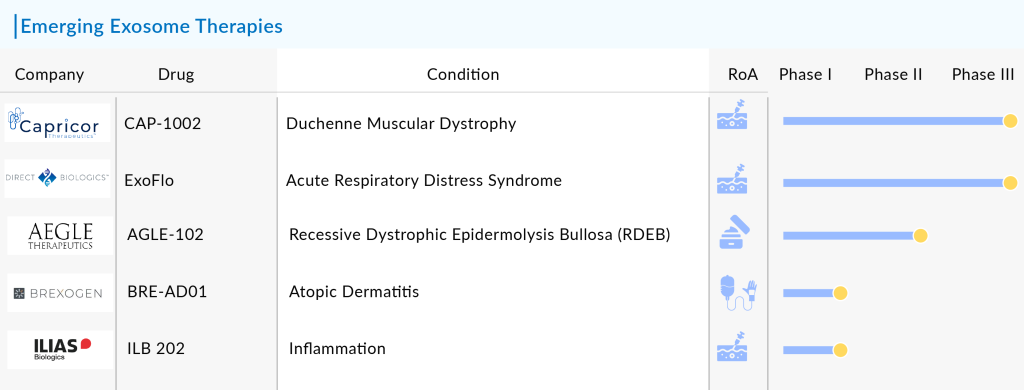
Brexogen’s BRE-AD01
BRE-AD01 is derived from stem cells known as ‘BxC,’ which are stimulated with a specific, clinically available compound that forms the basis of Brexogen’s technology. In various preclinical models, BRE-AD01 has shown superior therapeutic effects compared to competing treatments, including Dupixent, JAK inhibitors, and steroids.
The serious side effects have been reported in patients treated with JAK inhibitors, which were approved as innovative therapies for atopic dermatitis. In contrast, animals with atopic dermatitis treated with BRE-AD01 exhibited no side effects and demonstrated better therapeutic outcomes. BRE-AD01 operates through multiple mechanisms of action, including suppressing type 2 immune responses, modulating IL-31R, and enhancing skin barrier recovery, all of which contribute to improved symptoms of atopic dermatitis.
On October 27, 2022, the Center for Biologics Evaluation and Research (CBER) at the US FDA completed its review of the Phase I clinical trial for BRE-AD01 and confirmed the initiation of the trial. This marks the first Phase I clinical trial of therapeutic exosomes for atopic dermatitis in major countries. The approval of this Investigational New Drug (IND) application is significant, as it offers patients with atopic dermatitis the opportunity to receive improved treatment with BRE-AD01, which operates through multiple mechanisms of action.
ILIAS Biologics’ ILB-202
ILIAS’s lead program, ILB-202, is an exosome that carries the anti-inflammatory protein super-repressor IκB (srIκB) and is being developed for treating both acute and chronic inflammatory diseases. By introducing srIκB, the dominant active form of IκBα, the inflammatory responses in various disease models can be reduced, preventing the nuclear translocation of nuclear factor κB.
Unlike previous treatments that focus on upstream signaling pathways, ILB-202 minimizes the risk of off-target effects by directly targeting core inflammatory signals in the cytosol.
ILB-202 was investigated in a Phase I First-in-Human (FIH) clinical trial with a single ascending dose design to assess its safety, tolerability, immunogenicity, and pharmacodynamics in healthy volunteers. This double-blind, placebo-controlled study enrolled 18 randomized participants divided into three cohorts, with 12 receiving ILB-202 and 6 receiving a placebo.
Apart from these exosome-based therapies, some companies are also working with their candidates in the preclinical stage including EV Therapeutics (EV-101), Innovex Therapeutics (ExoCoVac), Coya Therapeutics (COYA 201), and others.
The anticipated launch of these emerging therapies are poised to transform the market landscape in the coming years. As these cutting-edge therapies continue to mature and gain regulatory approval, they are expected to reshape the exosome market landscape, offering new standards of care and unlocking opportunities for medical innovation and economic growth.
What Lies Ahead for Exosome-based Therapies?
Exosome-based therapies represent a promising frontier in regenerative medicine and targeted drug delivery, with the potential to revolutionize the treatment of various diseases, including cancer, neurodegenerative disorders, and cardiovascular diseases. As natural extracellular vesicles, exosomes facilitate intercellular communication and can carry proteins, lipids, and nucleic acids. This inherent ability to transport therapeutic molecules makes them an ideal candidate for targeted therapies. The future of exosome-based therapies will likely be shaped by advances in isolation and characterization techniques, enhancing our understanding of their biological roles and therapeutic potential. Additionally, innovations in engineering exosomes to enhance their stability and loading capacity could significantly improve their efficacy as drug-delivery vehicles.
Read our latest blog “Exosomes: Tiny Messengers with Big Potential in Medical Science” to get more insights on exosomes
Moreover, the integration of exosome-based therapies with cutting-edge technologies, such as CRISPR gene editing and nanotechnology, may open new avenues for precision medicine. The customization of exosomes for specific cellular targets, combined with their biocompatibility, offers the potential for minimizing off-target effects and improving treatment outcomes. Regulatory pathways for exosome-based products are evolving, with ongoing research aimed at establishing standardized protocols for their production and clinical application. As the scientific community continues to unravel the complexities of exosome biology, we can expect a surge in clinical trials and, ultimately, the adoption of exosome-based therapies in routine medical practice, offering new hope for patients with previously hard-to-treat conditions.

Downloads
Article in PDF
Recent Articles
- Kinase Inhibitors: Challenging the established Biologics as the new standard of care in autoimmun...
- Pfizer tightens DMD trial criteria over safety concerns; Kytopen raises $30M; Eli Lilly taps Reif...
- Wave Life Sciences stocks implode; Amarin’s VASCEPA approval; GSK seeks approval
- Zealand Pharma’s Phase III Results of Glepaglutide; FDA Approves Amylyx’s ALS Drug Relyvrio; Novo...
- Sarepta Therapeutics’s SRP-9001 Gene Therapy; FDA Approves Astellas’ VEOZAH; FDA Orphan Drug Desi...