AI in Cancer Diagnostics: Paving the Way for Early Detection and Precision Treatment
Nov 27, 2024
Table of Contents
Artificial Intelligence (AI) is revolutionizing numerous fields, and healthcare, particularly cancer diagnostics, is no exception. With the promise of faster, more accurate diagnoses, AI is transforming how clinicians detect, diagnose, and treat cancer. By leveraging vast amounts of medical data, advanced algorithms, and machine learning (ML), AI tools are helping doctors make more informed decisions, improve patient outcomes, and increase cancer care’s efficiency.
Discover how AI is revolutionizing patient care! Click to explore the Future of Healthcare with AI
Downloads
Article in PDF
Recent Articles
- Gilead and Merck Announce Encouraging Phase II Results of Islatravir and Lenacapavir Combo; REGEN...
- Top Five Liquid Biopsy Companies Impacting Cancer Diagnostics Market from 2020 to 2028
- Medical Odyssey: Solving the Dynamic Puzzle of Global Tourism Market
- Snippet
- Aerin Medical’s RhinAer Stylus; CE Mark for Haemonetics’s VASCADE Vascular Closure Device; J&...
Understanding AI’s Role in Cancer Diagnostics
Cancer is a complex and heterogeneous disease that manifests in various forms, affecting nearly every part of the human body. Early detection is critical for successful cancer treatment, as it significantly increases the chances of survival. However, traditional diagnostic methods—such as imaging, biopsy, and histopathological examination—often require a great deal of time and expertise, which can lead to delayed diagnoses and variability in results. AI offers an opportunity to augment and accelerate the diagnostic process.
AI in cancer diagnostics uses machine learning and deep learning algorithms to analyze vast amounts of data, including medical imaging (e.g., CT scans, MRIs, and mammograms), pathology slides, genetic data, and clinical records. These algorithms are trained to recognize patterns in the data, identifying potential signs of cancer that may not be visible to the human eye. In essence, AI can act as a powerful assistant to radiologists, pathologists, and oncologists, enhancing their ability to make more accurate and timely decisions.
Key Applications of AI in Cancer Diagnostics
AI is increasingly being applied across various aspects of cancer diagnostics, offering innovative solutions to enhance accuracy, reduce errors, and speed up the process of detection. By harnessing vast amounts of data and sophisticated algorithms, AI systems can assist clinicians in making more informed decisions. These tools not only improve the precision of cancer diagnoses but also facilitate personalized treatment plans, ultimately leading to better patient outcomes. Here are some of the key areas where AI is transforming cancer diagnostics:
Medical Imaging Analysis
AI’s role in medical imaging goes beyond simply detecting tumors. Modern AI algorithms can assess the subtle texture, shape, and growth patterns of tumors that might not be visible to the human eye. These algorithms can distinguish between benign and malignant growths with a high level of accuracy by learning from vast datasets of annotated images. AI systems can also monitor the progression of disease over time, helping clinicians track changes in the size and shape of tumors, offering insights into treatment effectiveness, and providing early indications of potential recurrence.
In addition to detecting tumors, AI in medical imaging can help with the classification of different types of cancer. For example, AI models are trained to differentiate between various subtypes of breast cancer, lung cancer, or brain tumors based on imaging characteristics. This classification is crucial as it impacts the treatment approach, with some subtypes responding better to certain therapies than others. AI can also prioritize cases based on the severity of the findings, assisting radiologists in making faster decisions in emergency settings.
Furthermore, AI systems can aid in identifying “false negatives” or overlooked abnormalities in routine screening, a major issue in cancer diagnosis. By improving the sensitivity of imaging techniques, AI helps reduce the chances of missing early-stage cancers, which can be critical in improving survival rates. As AI-powered tools continue to evolve, we can expect more advanced imaging systems that not only detect cancer but also provide real-time diagnostic suggestions for radiologists.
Finally, the use of AI in imaging is not confined to traditional diagnostic radiology but is expanding to include advanced modalities such as positron emission tomography (PET) scans and functional MRI. These scans offer detailed insights into the metabolic and functional activity of cancer cells, which AI can analyze to provide a more comprehensive view of the cancer’s behavior and its response to therapy.
Pathology and Biopsy Analysis
The process of diagnosing cancer from tissue biopsies has traditionally been time-consuming and dependent on the pathologist’s experience. AI’s ability to enhance digital pathology is helping address these challenges by providing a more standardized and efficient approach. AI tools can scan pathology slides, identifying cell patterns, nuclei shapes, and other microscopic features that may suggest cancerous changes. These tools can even detect minute abnormalities that might be too subtle for human detection, especially in cases of early-stage cancers or pre-cancerous lesions.
Additionally, AI models are becoming adept at quantifying cellular features such as tumor cell density, lymphocyte infiltration, and mitotic activity. These metrics can provide a more accurate picture of the cancer’s aggressiveness and potential for spread. This type of detailed, quantitative analysis aids pathologists in making more objective and precise diagnoses, which is especially important in cases with ambiguous or borderline findings.
AI’s ability to track the evolution of cancer at the cellular level is also proving useful for monitoring the effectiveness of treatment. By analyzing biopsies taken before and after treatment, AI can track changes in tumor biology, enabling oncologists to adjust treatment plans promptly. For instance, AI may identify changes in the tumor’s genetic makeup or detect the emergence of drug resistance, allowing for a more personalized approach to therapy.
Moreover, AI tools are helping to bridge the gap in regions with a shortage of trained pathologists. In areas where access to skilled medical professionals is limited, AI-powered diagnostic tools can assist in providing timely cancer diagnoses, ensuring that more patients receive the care they need. These systems also offer the potential for remote consultations, where pathologists can review digital slides from afar, expanding healthcare access globally.
Genetic and Molecular Profiling
AI is transforming the field of molecular diagnostics, which is a crucial component of precision medicine. Genetic profiling, such as DNA sequencing, allows for a deeper understanding of the molecular changes that drive cancer, but the sheer volume of data generated can be overwhelming. AI algorithms can rapidly process these vast datasets to identify key mutations, chromosomal abnormalities, and genetic markers associated with different types of cancer.
One notable advancement in this area is the use of AI in identifying actionable mutations, which are critical for selecting targeted therapies. For example, AI models can predict the response to treatments like tyrosine kinase inhibitors or immune checkpoint inhibitors based on the presence of specific mutations in the tumor’s genome. These models can also detect genetic changes that may predict a patient’s likelihood of developing resistance to certain drugs, helping clinicians adjust the treatment plan early to avoid ineffective therapies.
AI is also playing a role in identifying new biomarkers for cancer. By analyzing molecular data from large patient cohorts, AI can discover novel genetic or proteomic signatures that may not have been previously recognized, potentially leading to the development of new diagnostic tests or therapeutic targets. For instance, AI has been used to analyze RNA sequencing data to uncover cancer-specific gene expression patterns, offering insights into tumor behavior and potential therapeutic approaches.
Additionally, AI models can combine genetic data with other clinical information to provide a more comprehensive risk assessment for patients. For instance, integrating genetic mutations with lifestyle factors such as diet and exercise could help predict the likelihood of recurrence or metastasis, allowing for earlier interventions and better patient outcomes. As genomic data becomes more integrated into clinical care, AI will continue to be a valuable tool for delivering personalized cancer treatment.
Risk Assessment and Early Detection
AI-driven risk assessment tools have the potential to change the landscape of cancer prevention. These tools analyze a patient’s medical history, family history, lifestyle factors, and clinical data to calculate an individual’s risk of developing cancer. AI models can then provide a personalized risk score, which can guide clinicians in making preventive recommendations or determining the need for more frequent screenings.
For example, in the case of colorectal cancer, AI algorithms are being used to analyze patient records and determine who should undergo colonoscopies, based not just on age, but on a combination of genetic predisposition, lifestyle factors, and environmental exposures. This kind of early intervention could help identify high-risk patients before they develop the disease, leading to earlier, more successful treatment options.
AI is also being leveraged for the development of non-invasive screening tests. By analyzing blood samples, urine, or other bodily fluids, AI can identify subtle molecular signatures associated with early cancer stages. This approach could eventually lead to more widespread and accessible screening options that do not rely on invasive procedures like biopsies or imaging. Such liquid biopsy technologies, combined with AI, hold the promise of detecting cancers at much earlier stages, even before clinical symptoms appear.
Moreover, AI-based models are being developed to integrate multi-modal data from imaging, genetic testing, and lifestyle information to provide more comprehensive risk assessments. This approach helps clinicians identify high-risk individuals who may benefit from closer monitoring or preventive measures, including lifestyle modifications, chemoprevention, or prophylactic surgeries. By leveraging AI for risk prediction and early detection, healthcare providers can adopt a more proactive, rather than reactive, approach to cancer care, ultimately improving long-term patient outcomes.
Predicting Treatment Response
AI’s ability to predict how patients will respond to treatment is particularly valuable in oncology, where the choice of therapy is often complex and individualized. One of the challenges in cancer treatment is determining the optimal therapy for each patient, as tumors can vary widely in terms of their molecular characteristics and their response to drugs. AI helps by analyzing vast amounts of patient data, including clinical records, genomic information, and prior treatment responses, to predict which therapies are most likely to be effective.
For instance, in the case of breast cancer, AI models can analyze genetic and molecular data from a patient’s tumor to predict whether they will respond to specific chemotherapy regimens or whether a targeted therapy, such as a HER2 inhibitor, might be more effective. These predictive models can also be used to assess the likelihood of adverse side effects, allowing for a more personalized treatment plan that maximizes the chances of success while minimizing unnecessary toxicities.
Moreover, AI can help track patient progress throughout treatment. By continuously analyzing data from clinical trials, patient monitoring systems, and even wearable devices, AI systems can provide real-time feedback on how a patient is responding to treatment. This allows oncologists to make adjustments more quickly—switching therapies or altering doses to improve efficacy or reduce side effects.
AI is also playing a role in optimizing immunotherapy, a promising but sometimes unpredictable treatment option. By analyzing biomarkers, such as tumor mutational burden or PD-L1 expression, AI systems can predict which patients are more likely to benefit from immunotherapy, potentially sparing others from the side effects and costs of ineffective treatments. With its ability to synthesize large datasets and identify meaningful patterns, AI is helping make treatment choices more data-driven and patient-centered.
In the future, AI will likely play an even more prominent role in personalized medicine, as it continues to integrate data from a wide range of sources and enhance the ability to predict responses to novel therapies, improving the effectiveness of cancer treatments across diverse patient populations.
Explore the Future of Healthcare: See How AI Apps are Transforming Patient Care!
AI in Cancer Diagnostics: Market Dynamics and Key Companies
AI in cancer diagnostics is transforming the healthcare landscape, enabling faster, more accurate, and more personalized approaches to identifying and treating various types of cancer. The global market for AI-driven cancer diagnostics is witnessing significant growth, fueled by advancements in machine learning, deep learning, and computer vision technologies. These technologies help analyze medical imaging, genomic data, and patient records, improving the accuracy and efficiency of cancer detection. AI’s ability to process vast amounts of data in real time allows for the early detection of tumors, helping clinicians make timely treatment decisions. As a result, AI is becoming a key tool in both clinical practice and research.
Several factors are driving the growth of AI in cancer diagnostics. Increasing awareness of the potential benefits of AI in healthcare, such as reducing human error, enhancing diagnostic precision, and improving treatment outcomes, is accelerating its adoption. Moreover, the rising incidence of cancer worldwide, coupled with an aging population, is placing immense pressure on healthcare systems. AI can alleviate this burden by streamlining diagnostic workflows and providing support to medical professionals, especially in underserved regions with limited access to specialized expertise. The integration of AI tools into electronic health records (EHR) and telemedicine platforms is further enhancing their accessibility and effectiveness.
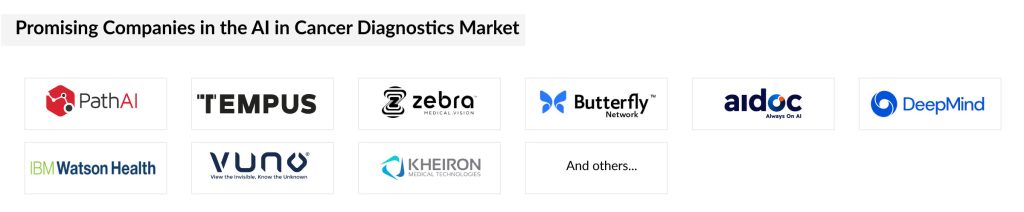
Key players in the AI cancer diagnostics market include technology giants like IBM, Google, and Microsoft, as well as specialized healthcare companies and startups. Companies like IBM Watson Health and Google Health are pioneering AI solutions in oncology, leveraging their vast computing resources to improve diagnostic algorithms. Additionally, startups such as PathAI and Zebra Medical Vision are developing cutting-edge AI-based tools focused on cancer imaging and pathology. These companies are collaborating with hospitals, research institutions, and pharmaceutical companies to expand their reach and validate their technologies. With continued investment and innovation, the AI in cancer diagnostics market is poised for significant expansion, offering new hope for earlier and more accurate cancer detection.
AI in Cancer Diagnostics: Challenges and Future Directions
While AI in cancer diagnostics holds tremendous promise, several challenges remain. Data quality and availability are critical to the success of AI algorithms. In many cases, medical data is fragmented, inconsistent, or not standardized, which can limit the accuracy and reliability of AI models. Furthermore, AI tools must be rigorously validated through clinical trials to ensure they meet regulatory standards and are safe for patient use.
There is also the issue of integration into existing clinical workflows. Although AI has the potential to enhance diagnostic accuracy, it must be seamlessly integrated with current medical practices, which can be a slow and complex process. Additionally, AI models must be interpretable and transparent, as clinicians need to understand how the algorithms reach their conclusions to trust their recommendations.
Despite these challenges, the future of AI in cancer diagnostics looks bright. Ongoing advancements in AI technologies, such as deep learning, natural language processing, and reinforcement learning, are expected to further improve diagnostic capabilities. Additionally, as AI models are exposed to larger and more diverse datasets, their accuracy and ability to generalize across different populations will continue to improve.
Downloads
Article in PDF
Recent Articles
- Colorectal Cancer Market Analysis and Market Forecast
- LensGen’s Juvene Intraocular Lens; Nevro announces clinical data publications; FDA Clearance to I...
- From Paper to Pixels: The Advantages and Challenges of Electronic Health Record
- Daiichi Sankyo’s Trastuzumab Deruxtecan; ODD to Bexmarilimab for AML; Roche’ Alecensa; Ergomed Ai...
- COVID-19 crisis can prove to be a catalyst for Artificial Intelligence in Healthcare