Exploring the Impact of AI in Mental Health: How it is Going to Revolutionize Diagnosis and Treatment for a Better Tomorrow?
Apr 23, 2025
Table of Contents
One in every eight people worldwide lives with a psychiatric disorder—a staggering statistic that underscores the deep and growing impact of mental illness on global health. The mental health crisis has evolved into a pressing public health emergency, fueled by increasing social pressures, lifestyle changes, environmental stressors, and limited access to care. From depression and anxiety to more complex conditions like bipolar disorder and schizophrenia, mental health disorders are affecting people of all ages, backgrounds, and geographies with increasing frequency and severity.
According to the World Health Organization, psychiatric and substance use disorders have surged by 13% in the past decade, reflecting not only rising prevalence but also persistent gaps in diagnosis, treatment access, and societal support. Despite the growing awareness, mental health care remains underprioritized in many regions, leaving millions untreated and underserved.
Downloads
Article in PDF
Recent Articles
- Vasomotor Symptoms of Menopause-Emerging Therapies
- Pressure Relief Devices: Charting the Course of Market Evolution and Major Developments
- Pancreatic Cancer Market Insights, Epidemiology and Market Forecast-2020
- Applications of AI in Healthcare: COVID-19 and Beyond
- AstraZeneca’s Tropion-Lung01 Phase III Trial Positive Outcomes; Biogen’s LEQEMBI South Korea Appr...
DelveInsight’s latest analysis across its core markets—the 7MM (the US, EU4, the UK, and Japan)—provides a more focused lens on this escalating crisis. In 2023, the diagnosed prevalent cases of schizophrenia in the 7MM were approximately 4 million, with the US alone accounting for around 1.4 million cases. Similarly, bipolar depression impacted nearly 3 million individuals, with about 70% of those cases reported in the US. Even more concerning, major depressive disorder affected nearly 44 million diagnosed individuals in the 7MM, making it one of the most common and debilitating mental health conditions.
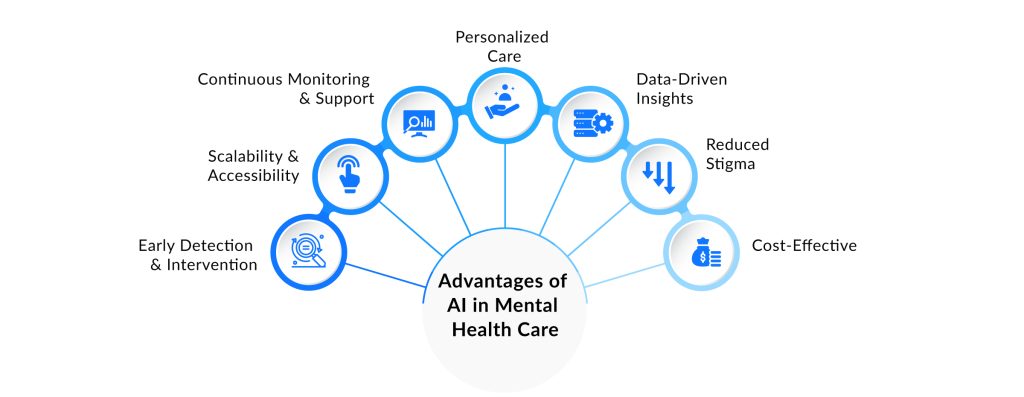
Pharmaceutical and biotech innovators are transforming mental health care by developing next-generation therapies, precision diagnostics, and digital interventions. These advancements, including AI-powered solutions, are crucial in enhancing mental health risk assessment, enabling personalized, accessible, and effective treatments. This progress is reshaping psychiatric care, offering hope to millions and driving a shift in how we approach mental health in the 21st century.
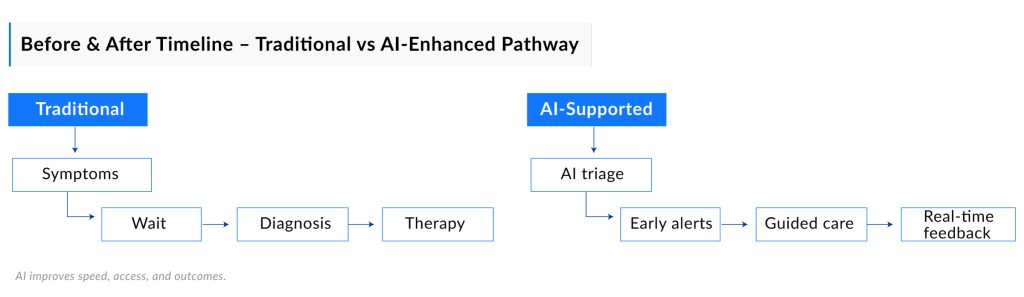
The Rising Role of AI in Mental Health
The use of AI in mental health care has grown significantly over the past decade. In 2015, only about 10% of mental health professionals used AI tools, mostly basic chatbots for stress relief, according to the American Psychological Association. By 2024, that number had risen to over 60%. Today’s AI systems are far more advanced, analyzing data like speech patterns or online activity to identify signs of depression or anxiety with up to 90% accuracy, as shown in a 2023 study in Nature Medicine. These advancements allow AI to offer timely, tailored support, helping people manage their mental health in ways that were once unimaginable.
AI is also making mental health care more accessible, especially where traditional resources are limited. Apps like Woebot and Wysa, which supported over 1 million users by 2022, offer cognitive behavioral therapy through AI-driven conversations that have evolved from text to voice-based interactions. Beyond individual support, AI is assisting clinicians by streamlining workflows, such as prioritizing patients who need urgent care. Hospitals using these tools have reported faster response times and better resource allocation. As AI continues to integrate with wearable devices, like smartwatches that monitor stress levels, it’s poised to transform mental health care into a more proactive, personalized field, ensuring help is available when and where it’s needed most.
Relevance of AI to Psychiatry and Psychology
Artificial intelligence is revolutionizing mental health care by enhancing diagnostics, treatment, and accessibility. Through advanced data analysis, AI leverages techniques like Natural Language Processing (NLP) to assess mental health risks by analyzing speech or text, identifying signs of depression, anxiety, or suicidal ideation. For instance, Ellipsis Health detects vocal biomarkers in patient conversations to flag potential risks. Machine learning models, such as those developed by IBM Watson Health, predict disorders like schizophrenia by analyzing genetic and neuroimaging data. Additionally, AI systems like Affectiva evaluate facial expressions and vocal tones during teletherapy, helping clinicians diagnose conditions like bipolar disorder with greater accuracy. Together, these AI applications are transforming how mental health conditions are identified and managed, improving care delivery while raising important ethical considerations.
Applications of artificial intelligence in psychology shine in personalized treatment, tailoring interventions to individual needs. AI-driven chatbots, such as Woebot, deliver cognitive behavioral therapy (CBT) for anxiety and depression, adapting responses based on user input to provide 24/7 support. In pharmacotherapy, AI in behavioral health predicts patient responses to medications; for instance, Tempus uses AI to analyze genetic profiles, reducing trial-and-error in prescribing antidepressants. AI-powered virtual reality therapy, like Oxford VR’s programs, creates immersive environments for exposure therapy, helping patients with post-traumatic stress disorder (PTSD) or phobias confront triggers effectively.
AI in mental healthcare significantly improves access to care, addressing barriers like cost, stigma, and clinician shortages:
- Telepsychiatry Support: Platforms like Ginger use AI to triage patients, connecting urgent cases with therapists swiftly.
- Multilingual Tools: AI-driven apps, such as Youper, translate mental health resources into multiple languages, serving diverse communities.
- Scalable Apps: Low-cost tools like Moodpath provide evidence-based interventions, enabling self-management of mild mental health issues.
In research, artificial intelligence and mental health intersect to accelerate discoveries. AI analyzes large datasets to uncover patterns, such as environmental impacts on mental health, as demonstrated by Google Cloud’s healthcare research tools. Deep learning interprets MRI scans to identify brain abnormalities linked to autism or Alzheimer’s, with companies like NeuroNet leading advancements. AI also streamlines clinical trials; for example, AiCure optimizes participant selection, cutting costs and timelines for psychiatric drug development.
Ethical challenges must be addressed to ensure the responsible use of AI in mental health:
- Bias: Algorithms trained on biased data may misdiagnose marginalized groups, as seen in early NLP models that underrepresented non-English speakers.
- Privacy: Sensitive patient data requires stringent safeguards, as breaches in apps like Talkspace have shown.
- Overreliance: Clinicians must balance AI in behavioral health tools with human empathy to maintain therapeutic rapport.
- Regulation: Unvalidated AI systems risk patient harm, necessitating rigorous testing, as emphasized by FDA guidelines.
AI in mental healthcare is reshaping psychiatry and psychology, making care more precise, personalized, and accessible. By integrating AI’s role in mental health risk assessment and scalable solutions, it empowers clinicians and patients alike. However, addressing ethical concerns like bias and privacy is crucial to ensure AI in behavioral health delivers equitable outcomes, solidifying its role in the evolving landscape of mental health care.
Role of AI in Diagnosis and Detection
Artificial intelligence is transforming mental health care by improving the accuracy and efficiency of diagnosis and detection. Through advanced algorithms and comprehensive data analysis, AI in mental health facilitates earlier identification of mental health conditions, enabling timely interventions and better patient outcomes. By leveraging machine learning, natural language processing, and predictive AI in mental healthcare is making mental health services more accessible and effective, particularly in underserved areas, while supporting clinicians with data-driven insights for more precise diagnoses.
AI is transforming healthcare diagnostics, from precision medicine to real-time monitoring. Explore our blog on AI in diagnostics and discover the latest advancements.
AI-powered Screening Tools
AI in mental health diagnosis is revolutionizing screening processes through innovative tools that analyze diverse data sources like speech, facial expressions, and text. Tools such as Limbic Access, a UK-based AI chatbot, screen for disorders like depression and anxiety with 93% accuracy, saving clinicians significant time per referral. Kintsugi, an American tool, detects vocal biomarkers in speech to identify depression and anxiety, addressing diagnostic gaps in primary care. Winterlight Labs uses speech analysis to detect early cognitive impairments, while Woebot, a CBT-based chatbot, identifies symptoms through text analysis, showing significant symptom reduction in trials. These AI in behavioral health tools enable scalable, non-invasive assessments, making mental health screening more accessible and efficient.
Mental Disorder Predictive Analysis Through AI
Mental disorder predictive analysis through AI is reshaping AI in mental health care by forecasting mental health conditions before symptoms fully emerge. By analyzing datasets like electronic health records, genetic data, and wearable metrics, AI in behavioral health identifies risk factors for disorders such as depression or schizophrenia. Vanderbilt University’s suicide prediction model uses hospital data to predict risk with 80% accuracy, while Cogito’s Companion analyzes voice patterns to alert care teams to crises. The Nature Medicine crisis prediction model forecasts mental health crises with high specificity, and Biobeat’s wearable technology predicts mood changes through physiological data. These advancements in AI for mental healthcare enable proactive, personalized interventions, which reduce disease severity and enhance patient care.
How AI is Being Used in Mental Health
AI in mental health is revolutionizing psychiatry and psychology, offering scalable, precise tools through applications of artificial intelligence in psychology and AI in behavioral health. As part of a broader exploration of AI’s impact on healthcare, AI in mental healthcare is examined through virtual therapists, mood and sentiment tracking, and predictive analytics for early detection. Real-world examples support this emphasis on AI’s role in mental health risk assessment. These advancements enhance care delivery while complementing human expertise.
Chatbots & Virtual Therapists
AI in mental healthcare drives chatbots and virtual therapists, delivering personalized, 24/7 mental health support. These tools utilize artificial intelligence and principles of mental health to provide cognitive behavioral therapy (CBT) and coping strategies tailored to individual needs. Woebot, a leader in AI for behavioral health, engages users in conversational CBT to manage anxiety and depression, analyzing responses to provide real-time feedback. Wysa’s multilingual chatbot supports AI in mental health by providing mindfulness exercises and emotional support, serving diverse populations. These tools reduce stigma and cost barriers, making therapy accessible via smartphones, with over 1 million users supported by such apps by 2022.
Mood and Sentiment Tracking
Mood and sentiment tracking leverages AI in mental health to monitor emotional states, strengthening AI’s role in mental health risk assessment. By analyzing text, speech, or behavioral data, AI identifies patterns linked to conditions like depression or anxiety. Ellipsis Health uses AI in behavioral health to detect vocal biomarkers in speech, assessing tone and word choice to flag mental health risks with 90% accuracy, per a 2023 Nature Medicine study. Youper’s NLP-driven app tracks sentiment through journal entries, helping users recognize emotional triggers and share trends with clinicians. This fosters self-awareness and supports early intervention for conditions like bipolar disorder.
Predictive Analytics for Early Detection
Predictive analytics in AI in mental healthcare forecasts mental health risks by analyzing genetic, neuroimaging, and behavioral data, enabling early detection. IBM Watson Health applies artificial intelligence and mental health to predict schizophrenia onset by identifying risk factors in genetic and imaging data. Mindstrong’s AI in mental health monitors smartphone usage, such as typing speed or app interactions, to detect depressive episodes early, facilitating proactive care. These tools shift applications of artificial intelligence in psychology toward prevention, reducing the burden of untreated conditions through timely interventions.
AI in mental health enhances care through innovative tools, with Woebot, Ellipsis Health, and Mindstrong showcasing the potential of AI in behavioral health. By integrating AI’s role in mental health risk assessment, AI in mental healthcare improves accessibility and precision. However, ethical challenges like data privacy and algorithmic bias must be addressed to ensure equitable impact within the evolving mental health landscape.
AI in Remote Monitoring
Artificial Intelligence is revolutionizing remote mental health care by enabling continuous, real-time insights into patient well-being—bridging the gap between clinical visits and everyday life. As questions like “can AI treat mental illness?” gain prominence, its role in remote monitoring suggests the answer may be evolving.
Mood & Vital Tracking via Wearables and Apps
The integration of AI in mental health with wearable devices and mobile apps is redefining how emotional well-being is monitored. These tools allow continuous tracking of physical and psychological markers—such as heart rate variability, sleep quality, and daily activity patterns—providing actionable insights into mental health status.
AI-powered apps like MoodKit, Youper, and Bearable use cognitive-behavioral strategies, mood journaling, and AI-driven analytics to help users track emotional patterns and receive tailored suggestions. MoodKit, for example, offers over 200 activities to improve your mood, while Youper leverages AI to facilitate conversations and detect signs of depression or anxiety. Bearable syncs with wearable devices like Fitbit or Apple Watch to combine physical and emotional data for a holistic view of well-being.
This data, analyzed through AI in mental healthcare, can help clinicians personalize care and detect subtle shifts that precede mood disorders or depressive episodes. By empowering users to monitor their mental health in real time, these technologies also improve engagement, reduce stigma, and support early intervention—answering “can AI treat mental illness?” with a growing body of supportive evidence.
Real-Time Risk Detection & Crisis Alerts
One of the most life-saving applications of AI in mental health is in suicide prevention and crisis intervention. AI systems can analyze changes in language, voice tone, or behavioral data from smartphones and wearable devices to flag high-risk individuals in real-time. These alerts can trigger timely interventions from clinicians or support networks—helping manage self-harm risks, substance abuse episodes, or psychotic breakdowns effectively.
AI-Powered Virtual Counseling
AI-driven platforms are also powering remote therapy through chatbots, virtual counselors, and telepsychiatry tools. These systems provide 24/7 support and can personalize sessions based on real-time mood data and patient history, enhancing engagement and reducing care gaps. Such innovations are reshaping access to therapy, especially in remote areas or for individuals reluctant to seek traditional in-person care.
In sum, remote monitoring powered by AI is making mental health care more proactive, personalized, and preventive—redefining how and when support is delivered.
Leading AI Tools and Companies in Mental Health
The integration of artificial intelligence into mental health care has led to the development of numerous innovative tools and platforms. These solutions aim to enhance diagnosis, treatment, and monitoring of mental health conditions, making care more accessible and personalized.
Prominent AI-Driven Mental Health Platforms
Several companies and their tools and wearables have emerged at the forefront of AI in mental health, offering a range of applications and services:
AI-Driven Mental Health Tools and Wearables:
- Happy Ring: Feel Therapeutics (FDA clearance, 2024)
A clinical-grade smart ring designed to monitor various health metrics, including sleep, blood oxygen, heart rate, activity, temperature, and brain activity. It integrates personalized machine learning algorithms and generative AI to provide actionable health insights, enabling coordinated clinical monitoring for conditions such as sleep apnea, heart disease, diabetes, obesity, hypertension, and more.
- Rejoyn: Otsuka & Click Therapeutics (FDA approval, 2024)
A prescription-only digital therapeutic smartphone app approved by the FDA for the treatment of major depressive disorder (MDD) in adults. It delivers cognitive behavioral therapy (CBT) through interactive tasks designed to rewire neural circuits associated with depression.
- EndeavorRx: Akili Interactive (FDA approval, 2020)
The first FDA-approved video game designed to treat Attention Deficit Hyperactivity Disorder (ADHD) in children aged 8–12. It employs game-based tasks to improve attention function.
- NightWare: NightWare Inc. (FDA clearance, 2020)
An FDA-cleared digital therapeutic system that uses an Apple Watch to monitor and intervene in PTSD-related nightmares by delivering gentle vibrations to disrupt nightmares without waking the user.
- Wysa: Wysa Ltd. (FDA Breakthrough Device Designation, 2022)
An AI-based digital mental health conversational agent that has received FDA Breakthrough Device Designation for its potential to assist in managing chronic musculoskeletal pain, depression, and anxiety through cognitive behavioral therapy delivered via a smartphone app.
- NeuroStar TMS Therapy: Neuronetics (FDA approval, 2008)
A transcranial magnetic stimulation (TMS) device approved by the FDA for the treatment of major depressive disorder in patients who have not benefited from antidepressant medications.
- BrainsWay Deep TMS: BrainsWay Ltd. (FDA clearance, 2013 for MDD; later expanded)
An FDA-cleared device that uses deep transcranial magnetic stimulation to treat depression and anxiety symptoms. It was later cleared for OCD in August 2018 and for smoking cessation in 2020.
- Prism for PTSD: Spark Biomedical (FDA clearance in US, 2024)
The first self-neuromodulation device to receive FDA clearance as a prescribed adjunct to standard care for PTSD, providing non-invasive brain stimulation to alleviate symptoms.
- Empatica’s Embrace2: Empatica (FDA clearance, 2018)
The world’s first medical-grade smartwatch to receive FDA clearance for neurological use, this wearable device is approved for seizure monitoring in epilepsy patients and also tracks physiological signals associated with mental health.
These approvals underscore the FDA’s recognition of the potential for AI and digital technologies to enhance mental health care through innovative therapeutic and monitoring solutions.

Drivers of AI in Mental Healthcare
Several factors are propelling the adoption of AI in mental health:
- Increased Demand: Rising mental health issues globally necessitate scalable solutions.
- Technological Advancements: Improvements in machine learning and natural language processing enhance AI capabilities.
- Data Availability: The proliferation of digital health data enables more accurate AI models.
- Cost Efficiency: AI solutions can reduce the burden on healthcare systems by providing cost-effective care options.
These drivers underscore the potential of AI to transform mental health care delivery.
Ethical Concerns and Challenges in Mental Health Care with AI
Data Privacy & Bias
The use of AI in mental health raises concerns about data privacy and algorithmic bias. Sensitive patient information must be protected to maintain confidentiality. Additionally, AI models trained on non-representative data may perpetuate existing biases, leading to disparities in care.
Replacing Human Interaction
While AI can augment mental health services, it cannot replace the empathetic connection provided by human therapists. Overreliance on AI may lead to a reduction in human interaction, potentially affecting the therapeutic relationship and patient outcomes.
Addressing these ethical considerations is crucial to ensure that AI serves as a beneficial tool in mental health care without compromising patient rights or care quality.
Recent Breakthroughs and Research Highlights in Mental Health and AI
As AI in mental health continues to evolve, groundbreaking research and technological advancements are redefining how we understand, diagnose, and treat psychiatric conditions. From predictive modeling and emotion-aware AI systems to wearable technologies and neurotherapeutics, recent innovations underscore AI’s expanding role in behavioral health and its potential to fill longstanding gaps in mental healthcare access and quality.
Below are some of the most notable developments that are shaping the future of AI in behavioral health and mental health diagnosis.
Stanford’s AI4MH Initiative
In April 2025, Stanford University launched the Artificial Intelligence for Mental Health (AI4MH) initiative, led by the Department of Psychiatry and Behavioral Sciences. This program aims to develop responsible AI tools tailored for psychiatric applications, facilitating their integration within clinical settings and fostering interdisciplinary collaborations. The initiative seeks to transform the research, diagnosis, and treatment of psychiatric and behavioral disorders through cutting-edge AI technology.
NeuroNOS’s BA-102 Receives FDA Orphan Drug Designation
In April 2025, NeuroNOS, a biopharmaceutical company focused on developing treatments for autism and Alzheimer disorders, and a subsidiary of Beyond Air (NASDAQ: XAIR), announced that the U.S. Food and Drug Administration (FDA) granted Orphan Drug Designation to its lead investigational therapy, BA-102, for the treatment of Phelan-McDermid Syndrome (PMS), a rare neurodevelopmental disorder linked to Autism Spectrum Disorder (ASD). The company plans to initiate first-in-human clinical trials for ASD in the United States in 2026.
AI Models and Emotional Responses
A study published in Nature in March 2025 revealed that large language models (LLMs) like ChatGPT can exhibit signs of anxiety when exposed to traumatic narratives involving accidents, military action, or violence. This elevated anxiety state impacts the AI’s subsequent responses and can amplify ingrained biases, affecting the reliability of the conversation. Researchers used the State-Trait Anxiety Inventory (STAI-s), typically used for human psychology patients, to measure AI anxiety. Mindfulness exercises, such as body awareness and calming imagery, were found to mitigate this anxiety, though not entirely reducing it to baseline levels.
Magstim’s Horizon Inspire System Gains FDA Clearance
In November 2024, Magstim, a global leader in neuroscience research and treatment for mental health, received FDA clearance for its Horizon Inspire System. This next-generation transcranial magnetic stimulation (TMS) technology is designed to treat patients with major depressive disorder (MDD), obsessive-compulsive disorder (OCD), and anxious depression. The system provides clinicians with advanced tools to deliver personalized TMS therapy, enhancing treatment efficacy and patient outcomes.
Happy Health’s Smart Ring Receives FDA Clearance
In October 2024, Happy Health, an innovative health technology company based in Austin, TX, received FDA clearance for its groundbreaking consumer-focused platform designed to bring clinical-grade healthcare directly into the home. At the heart of this platform is the Happy Ring—the first and only truly wearable medical device that seamlessly combines medical accuracy with all-day comfort. The ring monitors key health metrics such as sleep, blood oxygen, heart rate, activity, temperature, and brain activity, providing users with personalized health insights and enabling coordinated clinical monitoring.
The Future of AI in Mental Health: What’s Next?
As AI continues to redefine mental healthcare, the future promises even more transformative innovations. From AI-driven chatbots and virtual therapists to predictive analytics for early detection, artificial intelligence is not just enhancing care—it’s revolutionizing how we understand, diagnose, and treat mental health disorders. Tools like mood tracking apps, remote monitoring devices, and real-time crisis interventions are making mental health support more personalized, accessible, and proactive.
Companies at the forefront, such as Lyra Health, Woebot Labs, Talkspace, Spring Health, Wysa, Kintsugi Health, Ellipsis Health, Youper, Mindstrong, Happy Health, Rejoyn, EndeavorRx, NightWare, NeuroStar TMS Therapy, BrainsWay Deep TMS, Prism for PTSD, Empatica, and others demonstrate AI’s incredible potential to address the growing demand for mental health care, offering scalable solutions that complement human expertise.
However, the journey isn’t without its challenges. Ethical concerns surrounding data privacy, algorithmic bias, and the irreplaceable value of human empathy must be navigated carefully to ensure AI’s benefits are maximized without compromising care quality.
Looking ahead, the future of AI in mental health presents a landscape where AI will not only support but also enhance mental health ecosystems, moving us toward a smarter and more supportive mental health environment. As we continue to innovate, the role of AI in mental healthcare will undoubtedly evolve, enabling timely interventions, improving patient outcomes, and breaking down the barriers that have traditionally hindered access to care.
Downloads
Article in PDF
Recent Articles
- Baxter Introduced New Injectable Pharmaceuticals to US Market; Bayer and Hologic Collaborated to ...
- Norlase’s LYNX Receives FDA and CE Approval for Clinical Use; FDA Approves Imperative Care’s Zoom...
- Merck’s Antibody for Clostridium Difficile
- FDA Grants Priority Review to BMS’ Luspatercept; Teva and MedinCell’s Risperidone FDA Approval; B...
- FDA Approves Luye’s Rykindo; EU Approves AstraZeneca’s Tezspire; Oramed Announces Trial Results o...