Everything You Need to Know About Acute Kidney Injury
Jan 17, 2025
Table of Contents
Acute Kidney Injury (AKI) is a significant medical condition that affects millions of individuals worldwide each year. It is a rapidly progressive condition that requires timely diagnosis and treatment to prevent severe complications or long-term consequences. AKI is particularly prevalent in hospitalized patients, especially those receiving critical care, highlighting its global importance in healthcare settings.
What is Acute Kidney Injury?
Acute Kidney Injury (AKI) is a rapidly progressive condition that leads to a sudden decline in kidney function, typically over hours or days. It is characterized by the inability of the kidneys to effectively filter waste, manage fluid balance, and regulate electrolytes, which can result in serious complications such as electrolyte imbalances, fluid overload, and accumulation of toxins in the body. The causes of AKI are varied, including prerenal factors like decreased blood flow to the kidneys, intrinsic kidney damage, and postrenal obstruction in the urinary tract. Acute Kidney Injury can lead to permanent kidney damage if left untreated, but in many cases, the kidneys can recover with appropriate treatment.
Downloads
Article in PDF
Recent Articles
- NOTIZIA
- Reckitt Acquired Mead Johnson; LabCorp’s acquisition; Ferring collaborates; J&J Licenses
- FDA Grants Priority Review to Merck’s Application for KEYTRUDA Plus Padcev; Roche and Carmot Ther...
- BeiGene’s BRUKINSA Gets FDA Accelerated Approval; GSK’s Positive Results in DREAMM-8 ...
- Pooled Analysis of Finerenone Presented at EASD 2024, Poised to Strengthen its Position in the Ca...
Annually, AKI affects millions of people worldwide. Approximately 13 million cases of AKI occur globally, and although infections are a leading cause, they are more prevalent in low- and middle-income countries. In more developed nations, AKI is a common complication in hospitalized patients, especially in those in critical care. AKI can be classified into three stages, with Stage I being the mildest form and Stage III the most severe, often requiring acute kidney injury interventions like dialysis or renal replacement therapy (RRT). Treatment is mostly supportive, focusing on maintaining fluid and electrolyte balance, and preventing further kidney damage.
Symptoms of Acute Kidney Injury
The symptoms of AKI vary depending on the severity and the underlying cause. Early symptoms may be subtle, making it difficult to detect. However, as the condition progresses, symptoms become more noticeable and can include:
- Decreased Urine Output: A noticeable drop in the amount of urine produced.
- Swelling: Fluid retention leads to swelling in the legs, ankles, or face.
- Fatigue: Feeling unusually tired or lethargic.
- Shortness of Breath: Due to fluid accumulation in the lungs.
- Confusion: A result of the buildup of waste products in the blood.
- Nausea and Vomiting: Often caused by an imbalance in electrolytes.
- Chest Pain: This can occur if the kidneys fail to regulate fluid and electrolytes properly.
It is important to note that in some cases, AKI can be asymptomatic in its early stages. As a result, regular monitoring of kidney function is critical, particularly for patients at high risk.
Causes of Acute Kidney Injury
Acute Kidney Injury can result from various causes, which can be broadly classified into three categories:
- Prerenal Causes: These occur due to decreased blood flow to the kidneys, which can result from conditions like dehydration, heart failure, or severe blood loss.
- Examples: Hypovolemia, hypotension, heart failure, sepsis.
- Intrinsic (Renal) Causes: Damage to the kidney tissues, often caused by infections, toxins, or ischemia.
- Examples: Acute tubular necrosis (ATN), glomerulonephritis, interstitial nephritis.
- Postrenal Causes: These occur when there is an obstruction in the urinary tract that prevents the kidneys from filtering waste.
- Examples: Kidney stones, bladder obstruction, or tumors.
While infections are a common cause of AKI globally, it is important to note that infection-associated AKI is more prevalent in low- and middle-income countries. The risk of AKI is higher in individuals with certain underlying conditions like diabetes, hypertension, and heart failure.
Diagnosis of Acute Kidney Injury
Diagnosis of AKI typically involves blood tests, urine tests, and imaging studies. The main diagnostic criteria for AKI include:
- Serum Creatinine Levels: A sudden increase in serum creatinine by 0.3 mg/dL or more within 48 hours, or a 50% increase from baseline, indicates AKI.
- Urine Output: A reduction in urine output to less than 0.5 mL/kg/h for more than 6 hours suggests AKI.
- Urine Tests: To detect protein, blood, or other abnormalities that could indicate kidney damage.
- Imaging Studies: Ultrasound or CT scans to detect any physical obstruction or structural abnormalities in the kidneys.
Early-stage AKI may be asymptomatic, as clinical signs are contingent on the extent of renal impairment. Prioritizing the integration of kidney injury markers into clinical practice, as opposed to the current function-based approach, remains crucial for accurate diagnosis.
Stages of Acute Kidney Injury
AKI is classified into three stages based on severity, as defined by changes in serum creatinine levels and urine output:
- Stage I: A slight increase in serum creatinine (1.5-1.9 times baseline) or a decrease in urine output to less than 0.5 mL/kg/h for 6-12 hours.
- Stage II: A moderate increase in serum creatinine (2-2.9 times baseline) or a decrease in urine output to less than 0.5 mL/kg/h for more than 12 hours.
- Stage III: A severe increase in serum creatinine (3 times baseline or ≥4.0 mg/dL) or a decrease in urine output to less than 0.3 mL/kg/h for more than 24 hours, or the need for kidney replacement therapy.
In the U.S., Stage I comprised the highest number of AKI cases in 2023, with nearly 3.79 million cases, followed by Stage II. Stage III AKI, which often requires acute renal failure treatment, accounted for around 15% of cases.
Incidence and Impact of Acute Kidney Injury
Acute Kidney Injury affects millions of individuals worldwide. Globally, there are an estimated 13.3 million cases of AKI annually. The incidence of Acute Kidney Injury is higher in low- and middle-income countries, where infection-associated AKI is prevalent. The condition can occur at any age but is particularly common in elderly individuals, particularly those with multiple underlying health conditions. In the U.S., nearly 128K patients were admitted to the University of Florida Health, with 20% of encounters involving AKI.
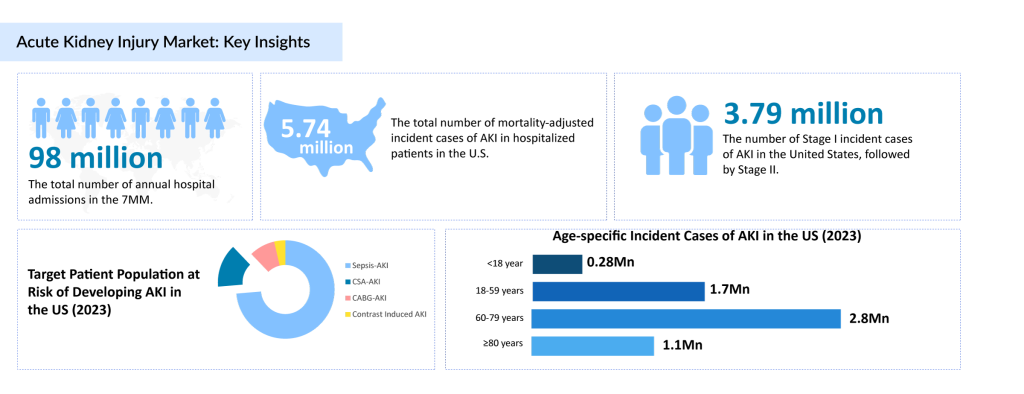
According to DelveInsight’s analysis, in 2023, the U.S. saw nearly 5.74 million mortality-adjusted incident cases of AKI in hospitalized patients. The overall incidence of AKI in hospitalized patients in the U.S. is around 9.57 million. In Germany, the highest number of AKI cases occurred in hospitalized patients, while France followed with a smaller share. In Japan, the age group of ≥ 80 years saw the highest number of AKI cases, followed by the 60-79 years age group. There is an unmet need to enhance the follow-up of individuals who have experienced in-hospital AKI episodes, as well as to identify those at risk of recurrent AKI or developing CKD.
which often requires acute renal failure treatment, accounted for around 15% of cases.
Treatment for Acute Kidney Injury
Currently, there are no specific pharmacotherapies approved for AKI treatment. Management of acute kidney failure is focused chiefly on supportive care, such as fluid resuscitation, electrolyte correction, and renal replacement therapy (RRT). RRT is necessary in severe cases, especially for those in Stage III of AKI. This therapy includes hemodialysis, peritoneal dialysis, and continuous renal replacement therapy (CRRT).
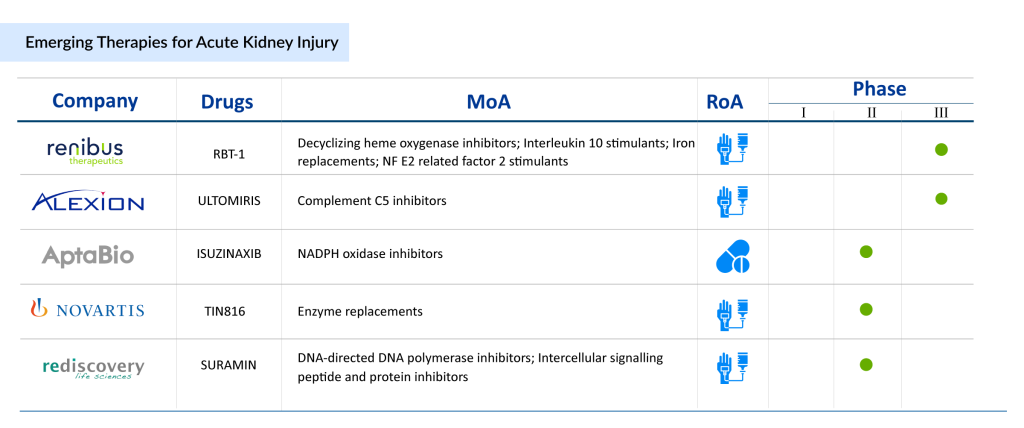
Apart from RRT, various off-label acute kidney injury medications are commonly used to manage AKI, including ACE inhibitors, ARBs, diuretics, and NSAIDs. However, these drugs only manage symptoms and are not targeted treatments for AKI itself. Several promising therapies are developing in the acute kidney injury pipeline, including RBT-1, Ilofotase alfa, and bRESCAP, which focus on mitochondrial function, reducing oxidative stress, and improving kidney recovery after injury. Furthermore, In January 2024, Renibus Therapeutics announced the publication of results from the Phase II Study evaluating RBT-1 as a preconditioning agent to reduce post-operative complications following cardiothoracic surgery. Also, In December 2023, SeaStar Medical announced enrollment of patients in the NEUTRALIZE-AKI pivotal clinical trial of its cell-directed Selective Cytopheretic Device (SCD) extracorporeal therapy in critically ill adults with AKI requiring continuous kidney replacement therapy (CKRT).
As of now, these therapies are in various stages of clinical development and hold promise for the future of AKI management.
To learn more about breakthrough therapies shaping the future of acute kidney injury treatment, click here!
Acute Kidney Injury Treatment Market Outlook
The market for AKI treatment is expected to grow significantly due to the increasing incidence of the disease and the evolving landscape of therapeutic options. According to DelveInsight, the AKI market was valued at USD 6.23 billion in 2022 across the 7MM and is expected to grow steadily during the forecast period (2024-2034). In the 7MM, the market is projected to grow at a CAGR of 4.1% from 2024 to 2034, with the U.S. being the largest contributor.
Acute Kidney Injury Treatment Market Trends and Insights
The market is driven by the increasing number of patients requiring renal replacement therapy (RRT) and off-label drugs, which include various classes such as ACE inhibitors, ARBs, Diuretics, and NSAIDs. These drugs are currently the primary form of treatment for severe AKI. With an aging population, rising rates of chronic diseases such as hypertension, diabetes, and heart failure, and increased recognition of AKI as a critical hospital-acquired condition, the demand for AKI treatments is set to grow.

Dive into our tailored blog to uncover the future of AKI treatment landscape—breakthrough therapies, emerging trends, and untapped opportunities
Acute Kidney Injury Treatment Market Barriers and Drivers
Acute Kidney Injury (AKI) remains a major healthcare challenge due to its sudden onset and severe consequences, including kidney failure and prolonged hospital stays. As healthcare systems grapple with the rising incidence of AKI, the market for treatments is evolving, driven by advancements in preventive care and the need for effective therapeutic options. However, significant barriers also hinder the development and availability of treatments, making AKI a critical area for innovation.
Market Drivers:
The AKI market is driven by the increasing focus on prophylactic treatments, which aim to prevent AKI in high-risk patients. These treatments can reduce the incidence of AKI, improving patient outcomes and lowering healthcare costs by avoiding expensive interventions like dialysis. This preventive approach is a major opportunity for healthcare systems. In addition, the advancement of biomarkers for AKI has the potential to accelerate drug development. By identifying specific biomarkers and combining them with machine learning models, clinicians can more accurately target at-risk patients, leading to earlier interventions and more effective therapies. This personalized approach to treatment is set to transform the AKI market.
Furthermore, the rising prevalence of risk factors such as diabetes, heart failure, and hypertension contributes to the growing demand for AKI treatments. As these conditions increase globally, more patients are at risk for AKI, creating a significant market opportunity. Researchers are also focusing on identifying AKI sub-phenotypes and developing treatments tailored to these groups, which may help address the critical unmet needs in AKI therapy.
Market Barriers:
Despite these opportunities, the AKI market faces significant barriers, with high trial failure rates being a primary challenge. Many promising drug candidates for AKI have failed in clinical trials, such as the Phase II AKITA trial of RMC-035 and the Phase III REVIVAL trial of ilofotase alfa. These setbacks slow progress in developing effective treatments. Currently, dialysis and supportive care are the only available options, neither of which address the underlying causes of AKI or prevent further kidney damage. This gap in curative therapies remains a critical unmet need.
Additionally, the complexity of managing AKI due to its varied causes and presentations makes it difficult to find one-size-fits-all treatments. AKI can be triggered by conditions like infections, heart failure, or diabetes, complicating diagnosis and treatment. The decline in the number of acute care beds is also a growing concern, as fewer specialized kidney units are available to treat AKI patients. This shortage strains healthcare systems, leading to delayed treatment and poorer outcomes. Addressing these challenges will be key to improving the AKI treatment landscape.
Conclusion
Acute Kidney Injury represents a formidable challenge in global healthcare, impacting millions annually and posing significant consequences for patients and healthcare systems alike. While the absence of targeted pharmacological therapies highlights a critical unmet need, advancements in acute kidney injury treatments and innovations in care are paving the way for a transformative future.
Today, the cornerstone of AKI management includes early diagnosis, meticulous fluid management, and treatment for AKI through renal replacement therapies. However, the landscape is shifting with the development of novel acute kidney injury medications, advanced diagnostics, and personalized strategies to enhance outcomes. Emerging biomarkers and prophylactic approaches are redefining how we approach the treatment of AKI, offering new avenues for intervention and improved patient care.
As the healthcare industry evolves, integrating cutting-edge technologies and a deeper understanding of disease pathways will be pivotal in revolutionizing acute kidney injury treatment. From mitigating risks in high-burden scenarios to enhancing recovery outcomes, the future of AKI management promises innovation, precision, and resilience. The journey to addressing this pressing healthcare challenge is well underway, offering hope and a brighter outlook for patients worldwide.
Downloads
Article in PDF
Recent Articles
- Oral Mucositis – A Common Cancer Therapy Adverse Reaction
- FDA Approves Neurocrine’s CRENESSITY for Congenital Adrenal Hyperplasia; Checkpoint’s UNLOXCYT Ap...
- Telemedicine: Can it be the future of healthcare?
- Infectious Disease and Vaccines Pipeline Reports
- FDA rejects BioMarin’s Valoctocogene Roxaparvovec; J&J inks $6.5B deal; Alzheon bags $...