Adrenal Crisis – The Hurdles in Diagnosis and Treatment
Feb 23, 2022
Table of Contents
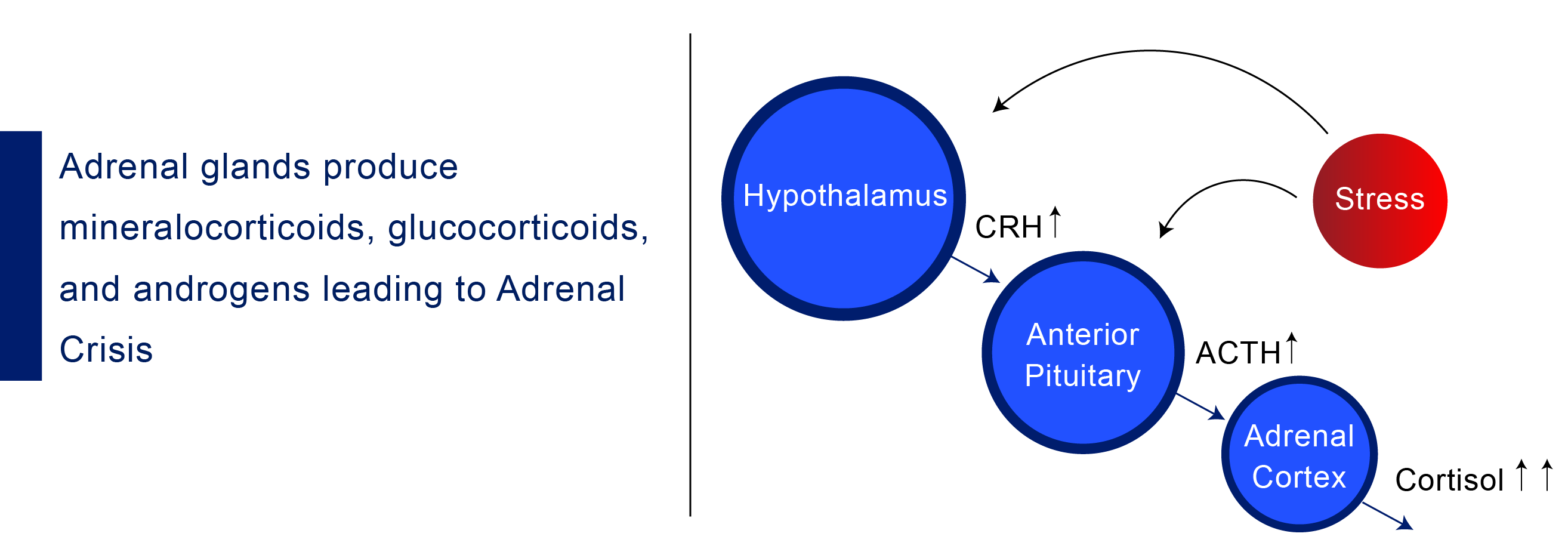
Adrenal Crisis refers to overwhelming and life-threatening adrenal insufficiency. The most common signs of Adrenal Crisis are shocking (very low blood pressure with a loss of consciousness), dehydration, and an imbalance of sodium and potassium levels in the body. In some cases, shock is then preceded by several other Adrenal Crisis symptoms such as fever, nausea, vomiting, abdominal pain, weakness or fatigue, and confusion. The standard Adrenal Crisis treatment is an instant infusion of hormone replacement therapy. Adrenal Crisis signs and symptoms usually occur after an infection, trauma, or another stressor.
An Adrenal Crisis most often occurs in a patient with known adrenal insufficiency (AI), either primary or secondary. Primary adrenal insufficiency (Addison Disease) is characterized by low cortisol and high ACTH from the destruction of the adrenal glands. Secondary adrenal insufficiency is characterized by low cortisol and low to normal ACTH caused by decreased ACTH secretion from the pituitary.
Downloads
Click Here To Get the Article in PDF
Recent Articles
The most common precipitating cause is acute infection (acute adrenal insufficiency), such as a gastrointestinal upset. Uncommonly, a patient will have no prior history or family history of autoimmune disease or adrenal insufficiency but will have acquired adrenal insufficiency due to chronic infection, such as from mycobacterium tuberculosis leading to chronic infectious adrenalitis and fibrosis, or have acute Meningococcal meningitis causing Waterhouse–Friderichsen Syndrome and massive bilateral adrenal hemorrhage.
Although a reliable diagnosis of underlying adrenal insufficiency is not possible during the initial period of fulminant Adrenal Crisis, a measurement of blood ACTH and cortisol during the crisis (before treatment with corticosteroids is given) is often enough to make a preliminary diagnosis. Providers should not delay treatment pending these results. Primary adrenal insufficiency (Addison disease) is characterized by low cortisol and high ACTH. Secondary adrenal insufficiency is characterized by low cortisol and normal ACTH.
Adrenal Crisis prevention necessitates adjusting hydrocortisone doses in response to stressful medical procedures (e.g., major surgery) and other stressful situations (e.g., infection). Patient education is critical for such dose modifications, but existing approaches are ineffective. As a result, better educational tactics are required.
The standard of care for Adrenal Crisis treatment is an instant infusion of hormone replacement drugs: hydrocortisone (an initial bolus of 100 mg IV or IM followed by 200 mg over 24 h or 50 mg IV or IM at every 6 h), 5% Dextrose containing solution (for hypoglycemia), IV Sodium chloride 0.9% (in hypovolemia condition), and antibiotics (if the patient has persistent symptoms of infection). The main goal of these Adrenal Crisis treatment medications is to revive normal cortisol levels in the patient and stabilize them.
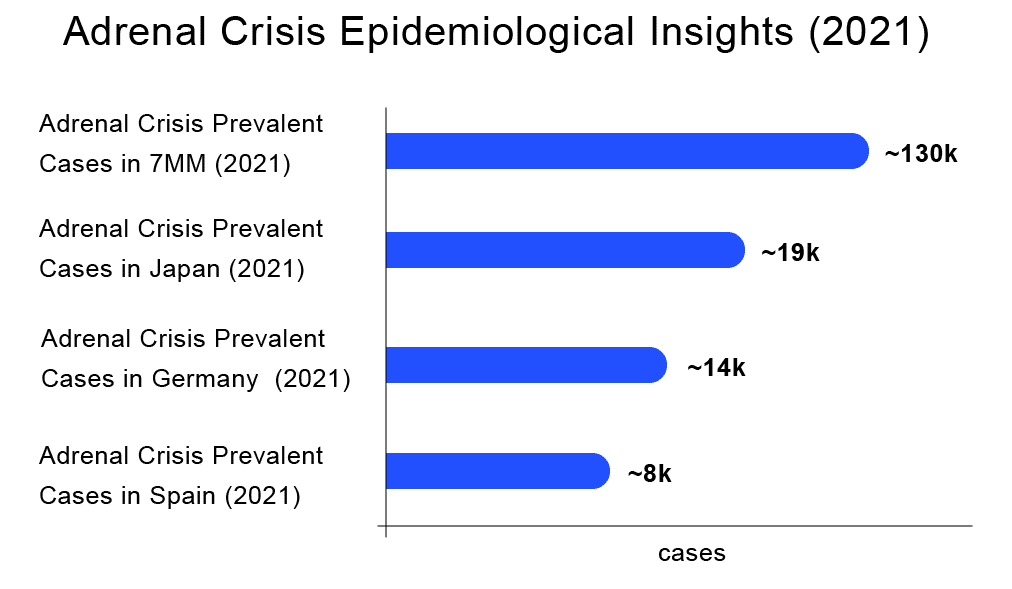
Adrenal Crisis Epidemiology
The total 7MM prevalent cases of the Adrenal Crisis were approximately 130,000 in 2021. The United States accounted for the highest number of cases, followed by EU5 countries and Japan. Japan had approximately 19,500 cases of Adrenal Crisis in 2021, as per DelveInsight’s assessments.
According to DelveInsight’s estimates, among the European countries, Germany had the highest number of prevalent cases of Adrenal Crisis (~14,700) in 2021 and is expected to decline to approximately 14,500 cases by 2032. At the same time, Spain had the lowest number of prevalent cases (~8,200) in 2021, which as per DelveInsight’s estimates, are expected to reach approximately 8,300 cases by 2032.
To determine the prevalent population of Adrenal Crisis in the 7MM (United States, Germany, France, Spain, Italy, United Kingdom, and Japan), we considered and compared data from various studies and organizational databases. Along with this, we also collected different KOL views and expert opinions to cover the geographical differences in Adrenal Crisis epidemiology across the 7MM.
Adrenal Crisis Market Scenario
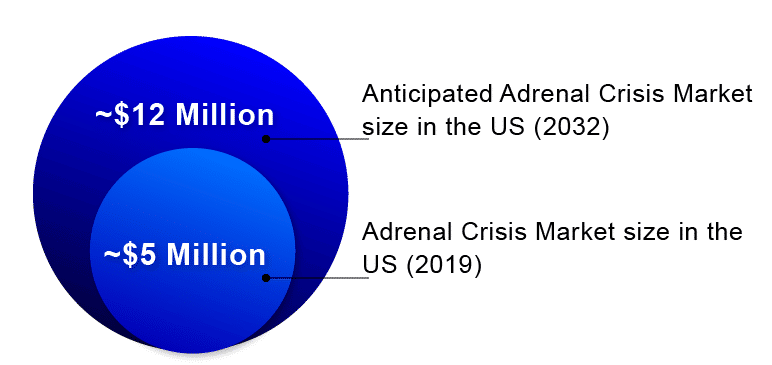
According to DelveInsight, the lion’s share of the Adrenal Crisis market remains with the United States throughout the forecast period (2019–2032).
The Adrenal Crisis market size in the US was ~USD 5 million in 2019 and is likely to generate close to USD 12 million by 2032.
In 2019, among EU5, Germany accounted for the largest market size (USD 1+ million), followed by France, the UK, and Italy with nearly 1 million each, whereas Spain accounted for the smallest share (~USD 0.7 million).
The future of the Adrenal Crisis market looks promising with emerging therapies such as ATRS-1902 (Antares Pharma) and Zeneo (Eton Pharmaceutical), among others.
Market leaders in the making
With a cornucopia of drugs in the pipeline, the Adrenal Crisis market size is projected to increase. Among the emerging therapies, the most promising ones include ATRS-1902 (Antares Pharma) – a Drug-Device Combination product, Zeneo (Eton Pharmaceutical) – a Drug-Device Combination product, among others.
Expected roadblocks
Despite the presence of gold standard hormone replacement therapy, around 40% of adrenal insufficiency patients still encounter acute adrenal insufficiency episodes at least once. Adrenal Crisis is documented to be life-threatening and lead to enormous economic burden due to emergency admissions and in-hospital care requirements, representing gaps in the market. This section discusses the unmet needs in the Adrenal Crisis market.
Adrenal Crisis Evaluation Data
The Adrenal Crisis remains one of the leading causes of mortality in adrenal insufficiency patients despite the availability of hormone replacement therapy. It has become increasingly evident that, even in patients with treated adrenal insufficiency, there continues to be significant morbidity due to the need for a high dose of IV hydrocortisone during acute episodes. Recent data from the European Adrenal Insufficiency Registry (including both PAI and SAI patients) found the major causes of death in patients with adrenal insufficiency were cardiovascular disease (35%) and infection (15%), supporting previous registry data for patients with PAI. The EU-AIRE study reported a mortality of 1.5% for patients with SAI. In those patients with SAI who died, 11.1 Adrenal Crisis cases per 100 patient-years were reported, significantly higher than reported in other cohorts of patients with SAI. In addition, patients with SAI who died were on higher mean daily doses of hydrocortisone (24.0 ± 7.6 versus 19.3 ± 5.7 mg, p = 0.002), which may reflect the physicians’ response to repeated adrenal crises, with increased doses of glucocorticoid therapy in an attempt to prevent recurrence of Adrenal Crisis. In addition, patients with SAI who died were on higher mean daily doses of hydrocortisone (24.0 ± 7.6 versus 19.3 ± 5.7 mg, p = 0.002), which may reflect the physicians’ response to repeated Adrenal Crisis, with increased doses of glucocorticoid therapy in an attempt to prevent recurrence of Adrenal Crisis.
Acute Adrenal Crisis can swiftly proceed from nonspecific symptoms such as fatigue and nausea to a life-threatening condition such as hypovolemic shock. The availability of hormone replacement therapy at the right moment is critical in treating these patients. All of the approved Adrenal Crisis treatments, however, are in the form of injections and require reformulation or IV/IM delivery. Over two-thirds of adrenal insufficiency patients, according to research, rely on medical personnel for first-line emergency treatment (4% ambulance workers, 23% GP/nurse, and 38% hospital employees) because the available medication is difficult to administer. As a result, a self-administered hormone replacement injectable that is readily available during times of crisis is critical.
Adrenal Crisis Facilitations and Diagnostic Hurdles
There are currently no reliable laboratory tests or other bio-markers to adequately predict the probability of an incumbent Adrenal Crisis. Hence it remains a challenge for the endocrinologist to identify individual patients with increased vulnerability. Therefore, clinical tools are needed to detect individuals at increased risk and, ideally, detect prodromal periods of an Adrenal Crisis, enabling the clinician to interfere timely and prevent progression into an overt crisis.
A recent study investigated the role of longitudinal disease-specific QoL questionnaires (i.e., AddiQoL) in Adrenal Crisis diagnosis of prodromal periods. This study shows that score deviations in longitudinal AddiQoL assessments may help patients detect their risk of an Adrenal Crisis and thereby identify patients at increased risk of Adrenal Crisis. Other diagnostic tools for predicting an Adrenal Crisis or detecting its prodromal symptoms are needed for targeted Adrenal Crisis treatment. Other diagnostic tools for predicting or detecting Adrenal Crisis prodromal symptoms are needed for targeted treatment.
Adrenal Crisis is multifactorial as it can be caused by primary AI, secondary AI, tertiary AI or due to other reasons such as vomiting (unable to take oral hydrocortisone), infection, or trauma (need for cortisol increases due to external factors leading to a gap between necessity and availability). Adrenal Crisis symptoms are variable such as hypotension and hypovolemia (in patients with PAI due to concomitant mineralocorticoid deficiency), but patients often have nonspecific symptoms, such as anorexia, nausea, vomiting, abdominal pain, fatigue, lethargy, fever, or altered consciousness. The insidious onset of symptoms often results in a delay in Adrenal Crisis diagnosis. A research study of Adrenal Crisis admissions reported that 66.9% of Adrenal Crisis patients (n = 337) had visited the hospital within 90 days before the onset of the crisis. Hypotension (particularly postural hypotension) occurs secondary to hypovolemia but also due to hypocortisolism. Hence, if adrenal insufficiency is not suspected, it may be refractory to parenteral fluids and inotropes. In PAI, hyponatremia and hyperkalemia can occur due to mineralocorticoid deficiency. Other biochemical features that can present in an Adrenal Crisis include renal impairment secondary to hypovolemia, hypoglycemia, and, rarely, hypercalcemia, which is due to decreased renal excretion of calcium and increased bone resorption.
The conventional hormone replacement strategies do not mimic physiological hormonal secretion patterns, and, since many factors are known to affect individual glucocorticoid sensitivity (i.e., other medications, glucocorticoid receptor polymorphisms), it remains difficult to establish an optimal replacement dose for the individual patient. Insufficient cortisol coverage results in chronic noradrenergic activation with many complaints and the risk of a potentially fatal Adrenal Crisis during increased stress, whereas even subtle glucocorticoid overexposure results in a Cushing-like phenotype with higher hydrocortisone levels being associated with impaired QoL. In agreement with this finding, the adverse metabolic, cardiovascular, and psychological effects of long-term supraphysiological glucocorticoid replacement need specific attention since there are significant associations between chronic over replacement and diabetes mellitus type 2, obesity, osteoporosis, psychological morbidity, maladaptive personality traits, and premature cardiovascular death, respectively. Some novel treatment advances to meet the need of matching circadian rhythm are modified-release hydrocortisone oral medications (Plenadren); however, they do not serve high dose requirements during acute attacks.
Adrenal Crisis Future Updates
As per DelveInsight’s estimates, the Adrenal Crisis treatment market landscape looks promising, studded with remarkable advances in diagnosis and treatments that will translate into a better quality of life and improved survival. The entry of the novel Adrenal Crisis therapies to attain better healthcare will necessitate collaboration among academia, life-sciences companies, funding, regulatory agencies, decision-makers, and caregivers. In addition, expertise in navigating market access and reimbursement scenarios would be an elixir to devise successful GTM strategies for new therapies.

FAQs
An Adrenal crisis is a life-threatening condition that occurs when there is not enough cortisol. This is a hormone produced by the adrenal glands in the body.
Each year roughly 8% of those with known adrenal insufficiency have an Adrenal Crisis, and the rate of death is around 6%.
Adrenal Crisis is extremely serious and can cause death if not treated promptly.

Downloads
Article in PDF