How are Antipsychotics Transforming the Schizophrenia Treatment Space?
Oct 18, 2024
Table of Contents
Schizophrenia affects approximately 24 million people worldwide, or 1 in every 300 people (0.32%). In adults, this rate is 1 in 222 (0.45%). It is not as widespread as many other mental disorders. Onset occurs most frequently in late adolescence and the twenties, and it occurs earlier in men than in women.
Schizophrenia is frequently associated with significant distress and impairment in important areas of life such as personal, family, social, educational, occupational, and other. People with schizophrenia are twice as likely as the general population to die young. This is frequently due to physical illnesses such as cardiovascular, metabolic, and infectious diseases.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- US/AZ deal; Alkermes’ Schizophrenia drug; Innovent/Lilly’s China market expansion; Re...
- Exploring the Impact of AI in Mental Health: How it is Going to Revolutionize Diagnosis and Treat...
- Hope on the Horizon: Brilaroxazine’s Promise for Schizophrenia Patients
- Breaking Boundaries: Innovations and Updates in Schizophrenia Treatment
- Acquisition of Stemline; Roche’s Elecsys Anti-SARS-CoV-2 antibody test; Newron’s abandonment of S...
According to DelveInsight’s 2023 analysis, the schizophrenia prevalence across the 7MM reached around 4 million diagnosed cases, with the US accounting for 1.5 million. In the EU4 and UK, cases were further divided by severity, with severe accounting for the highest number of cases. Looking ahead, global advancements in psychiatric research and diagnostics are anticipated to boost precise schizophrenia identification by 2034.
A person with schizophrenia can have symptoms like delusions, hallucinations, disorganized speech, trouble with thinking, and might feel demotivated. It is a disorder with variable phenotypic expression and poorly understood, complex etiology, involving a major genetic contribution, as well as environmental factors interacting with the genetic susceptibility.
Despite its antiquity, most of what is known about schizophrenia has been discovered over the past 10 decades, mostly in the late twenties and early twenty-first centuries. A lot of research has been going on to give a clearer picture of the illness. However, despite a century of research, the pathophysiology of schizophrenia remains elusive.
Diagnostic scales, which have been extensively validated, are widely used within clinical practice and research settings. Two key examples include the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM) and the World Health Organization’s International Classification of Diseases (ICD).
Both the DSM, for which at least two schizophrenia symptoms including delusions, hallucinations, disorganized speech and behavior, and negative symptoms need to have been present for at least six months and for a significant portion of time over one month, and the ICD for which at least two schizophrenia symptoms must be present, including positive, negative, depressive, manic, psychomotor, and cognitive symptoms. Of the two schizophrenia symptoms, one core symptom needs to be present. Schizophrenia symptoms should have been present most of the time during a period of at least one month. These criteria are regularly updated, and the most recent versions are the DSM-5 and the ICD-11.
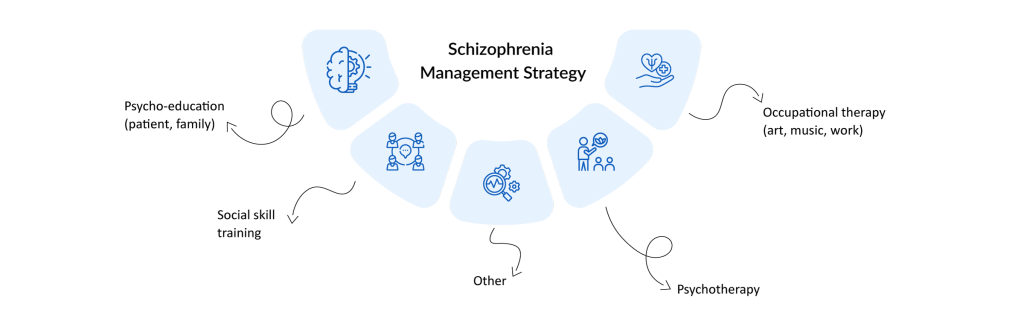
Schizophrenia Multimodal Treatment Strategy
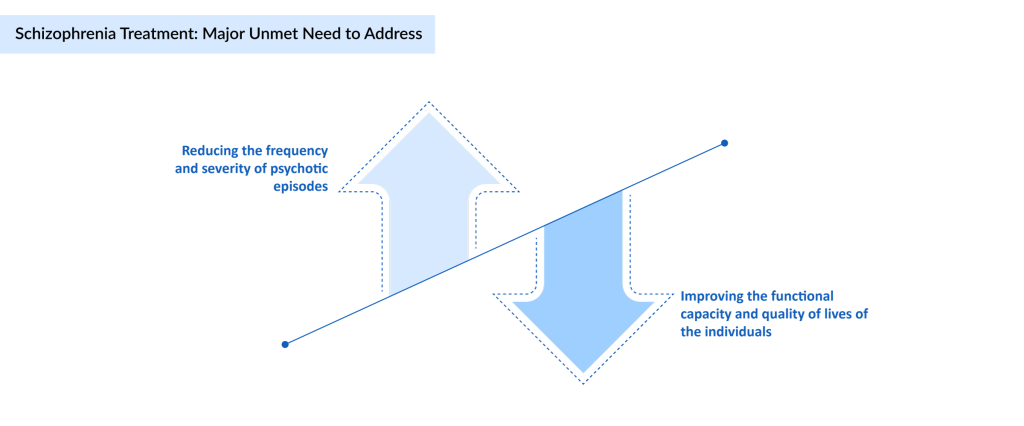
Despite therapeutic advancements in recent decades, schizophrenia remains one of the most severe mental illnesses, with a chronic relapsing course and significant functional impairment in a significant number of individuals. Currently, there is no cure for schizophrenia. However, the disorder is treated and manageable with a combination of schizophrenia therapies. Although the aim of treatment of schizophrenia varies depending on severity and phase, but the short-term primary goal of schizophrenia treatment is to control symptoms. The primary goal is to manage psychotic symptoms and enhance patients’ quality of life (QoL). However, the long-term objective of treatment of schizophrenia is to achieve stability and avoid sickness return.
The Goal of Schizophrenia Treatment
The current pyramid of interventions in managing schizophrenia includes antipsychotic medications, the most commonly prescribed schizophrenia drugs and thought to control symptoms by affecting the brain neurotransmitter dopamine. Even after symptoms have faded, schizophrenia requires lifetime therapy. Apart from schizophrenia medications, psychological counseling, and social support, cognitive behavioral therapy and electroconvulsive therapy (ECT) can be used to control the condition. Hospitalization may be required in some circumstances.
Schizophrenia treatment is generally guided by a psychiatrist with expertise in treating schizophrenia, including a psychologist, social worker, or psychiatric nurse. Although therapy objectives such as response, remission, and recovery have become more generally defined, a reliable “effectiveness” metric that maps onto functional outcomes remains missing. Furthermore, the field must progress in translating measurement-based techniques from research to clinical practice. Adding to this debate is continuous disagreement about whether first-generation or second-generation antipsychotics should be used.
Key Differences Between First and Second Generation Antipsychotics
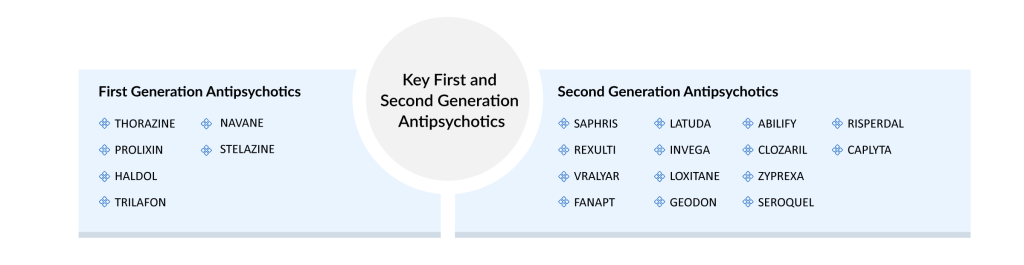
Antipsychotics (APs) are the first-line treatment for schizophrenia on the market. These are divided into two categories: first-generation antipsychotics (FGA; or conventional APs) and second-generation antipsychotics (SGA) (SGA; or atypical APs). Both first and second-generation antipsychotics differ significantly in their pharmacological profiles and side effects.
First-generation antipsychotics (FGAs), also known as typical antipsychotics, primarily block dopamine D2 receptors, effectively reducing positive symptoms like hallucinations and delusions, but often cause extrapyramidal side effects such as tremors and rigidity. Second-generation antipsychotics (SGAs), or atypical antipsychotics, act on both dopamine and serotonin receptors, providing relief from both positive and negative symptoms with a lower risk of motor side effects.
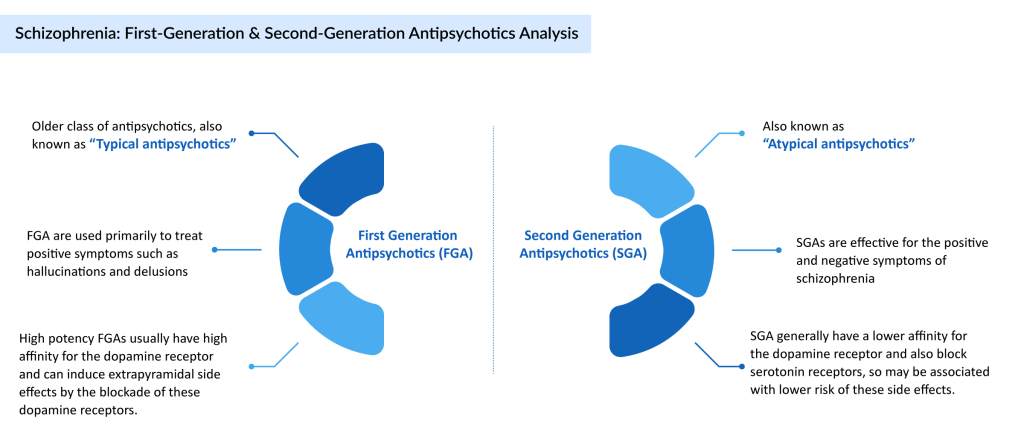
These are either administered orally for oral antipsychotics (OAP) or intravenously for long-acting injectable treatment for schizophrenia. Although both first and second-generation antipsychotics are used for schizophrenia treatment, the usefulness of the second generation over the first is controversial, as is the effectiveness of LAI over OAP.
However, when evaluating individual adverse effect profiles, the distinction between first and second-generation antipsychotics as unified classes cannot be maintained, requiring a more differentiated approach and schizophrenia treatment decision. The intended, tailored schizophrenia treatment strategy must take present symptoms, comorbid diseases, previous therapeutic responses, adverse effects, and patient preference and expectations into account.
Today, at the global level, some of the key companies, such as Boehringer Ingelheim, Sumitomo Pharma, Otsuka Pharmaceuticals, Reviva Pharmaceuticals, Minerva Neurosciences, Mitsubishi Tanabe Pharma, Karuna Therapeutics, Bristol Myers Squibb, Royalty Pharma, Acadia Pharmaceuticals, Rovi Pharmaceuticals Laboratories (Laboratorios Farmacéuticos Rovi), Teva Pharmaceutical, MedinCell, Lyndra Therapeutics, Neurocrine Biosciences, Luye Pharma, Newron Pharmaceuticals, and others, are evaluating various new antipsychotics in different schizophrenia clinical trials to improve the treatment space.
Currently, the therapies in the schizophrenia pipeline include IIclepertin (BI-425809), Ulotaront (SEP-363856), Brilaroxazine (RP5063), Roluperidone (MIN-101/MT-210), KarXT (xanomeline-trospium), NUPLAZID (pimavanserin), OKEDI/RISVAN (risperidone ISM), Olanzapine LAI (mdc-TJK/TV-44749), Valbenazine (NBI-98854), LYN-005 (long-acting oral risperidone), Evenamide (NW-3509), LY03010 (ER paliperidone palmitate), and others. The launch of these schizophrenia treatment medications in the coming years will significantly improve people’s lives affected by schizophrenia.
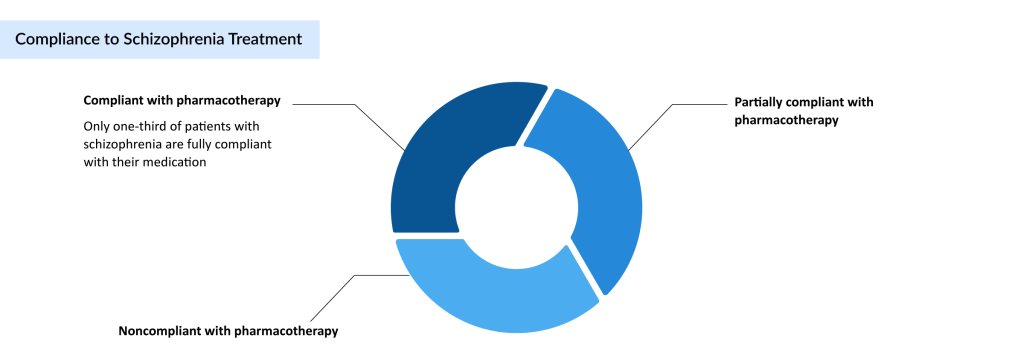
Moreover, the global prevalence of schizophrenia has observed stable growth in the past two decades, and the same stable growth is expected in the coming years. Governments and health organizations must raise awareness to make schizophrenia patients comfortable to combat mental illness and raise awareness of the long-term repercussions. However, due to the side effects of the antipsychotic schizophrenia medication, compliance is quite less, and it is a challenge for the caregivers to tackle this issue. Despite antipsychotic therapy, schizophrenia is linked with considerable unmet medical demands, functional impairments, and a high burden of illness. One of the biggest impediments to treatment effectiveness in schizophrenia is medication non-compliance. Non-adherence is prevalent, with outcomes including insufficient symptom management, relapse, hospitalization, and increased consumption and expense of health care resources.
Compliance of Schizophrenia Patients
Schizophrenia patients who stop using antipsychotic medications maybe two to five times are more likely to relapse than other schizophrenia patients. Although the causes for medication non-adherence are varied, the failure to stay on schizophrenia medicine jeopardizes the chance of remission and better functioning in people with schizophrenia. To date, clozapine is the only evidence-based treatment for refractory schizophrenia patients, and the role of antipsychotic polypharmacy and other augmentation strategies remains unclear at best.
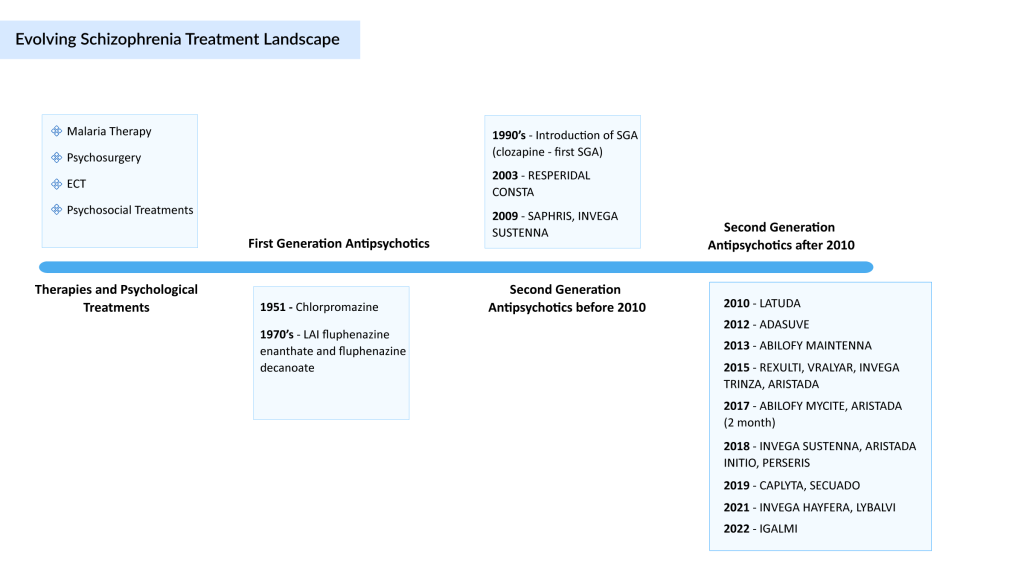
Schizophrenia Treatment Landscape
To discover novel schizophrenia treatment medication with enhanced/broader efficacy and improved tolerability, and to enable personalized treatment, the mechanisms underlying illness development and progression, symptomatic improvement, and side effect development need to be elucidated. Most people with schizophrenia benefit from combined antipsychotic medication and non-pharmacologic treatments that address their personal goals. Several promising approaches for improving outcomes in schizophrenia are under study that may help mitigate persistent psychotic symptoms, negative symptoms, and cognitive deficits in patients with established illnesses. Attention is being focused on the early administration of psychosocial interventions to reduce persistent disability.
Nevertheless, after over a century of schizophrenia treatment, significant progress has been made, starting from the lobotomy operations, through the discovery of chlorpromazine, to current second and third- generation antipsychotics. Novel approaches, following new studies in the disease mechanisms, will finally result in a new generation of schizophrenia drugs.
As per DelveInsight analysis, the schizophrenia market size in the 7MM is expected to change during the study period (2020–2034). In 2023, the total schizophrenia market size was USD 8 billion, which is expected to rise by 2034.
Furthermore, the WHO’s Comprehensive Mental Health Action Plan 2013–2030 will raise mental health awareness by ensuring that 100 million more people have access to quality and affordable mental health care.
Downloads
Article in PDF
Recent Articles
- Vanda Broadens its Reach to Bipolar Disorder Treatment Market With Fanapt Approval
- Horizon, Viela Deal; Concert Schizo Drug Flop; Gilead Deals with Arcus and Gritstone
- Evenamide (NW-3509): Advancing Solutions for Treatment-Resistant Schizophrenia
- Breaking Boundaries: Innovations and Updates in Schizophrenia Treatment
- BioXcel’s Agitation Drug Igalmi; FDA Approves Cysteine Hydrochloride Injection; Gilead’s Trodelvy...