6 Groundbreaking Applications of Organoids That Are Changing Healthcare
Nov 06, 2024
Table of Contents
The advent of organoid technology has marked a revolutionary milestone in biomedical research and healthcare. Organoids, which are three-dimensional structures derived from stem cells that mimic the architecture and functionality of specific organs, have opened new avenues for understanding diseases, testing drugs, and advancing personalized medicine.
6 Applications of Organoids in the Healthcare Landscape
Organoids are revolutionizing healthcare by offering a glimpse into the future of personalized medicine. These miniature, lab-grown versions of organs replicate key functions and structures, enabling researchers to study disease mechanisms, test drug efficacy, and tailor treatments to individual patients. From cancer research, where organoids help unveil tumor behavior and treatment responses, to regenerative medicine, where they pave the way for organ replacement, the applications are vast and transformative.
Downloads
Article in PDF
Recent Articles
- Amgen to Purchase Horizon Therapeutics; IND Clearance to Vertex’s VX-522; FDA Fast-Track Designat...
- The lab-grown mini-brains generate electrical patterns
- Lack of effective therapy: A major Nontuberculous Mycobacteria Infection Market Driver
- Alarming Growth of Chronic Respiratory Diseases (CRDs) and Their Prolonged Impact on the Quality ...
- FDA approval to AZ’s Farxiga for heart failure; GSK divests two travel vaccines to Bavarian Nord...
Read our latest article “Tiny Organs, Big Impact: How Organoids are Shaping the Future of Medicine” to learn more about organoids
By bridging the gap between traditional cell cultures and actual human tissues, organoids hold the promise of more accurate models for testing therapies, ultimately leading to better patient outcomes and advancing our understanding of complex diseases. Let’s delve into the 6 key applications of organoids that are changing the healthcare landscape.
Disease Modeling with Organoids
Disease modeling using organoids has emerged as a transformative approach in biomedical research, enabling scientists to recreate complex disease states in vitro. By deriving organoids from patient-specific stem cells, researchers can mimic the architecture and cellular diversity of actual tissues, which facilitates the study of various diseases, including genetic disorders, infections, and degenerative conditions. For example, intestinal organoids can model inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis, allowing for the exploration of disease mechanisms and the testing of new treatments in a controlled environment.
This level of realism helps bridge the gap between traditional two-dimensional cell cultures and the intricate cellular interactions found in living organisms, providing deeper insights into the pathology and progression of diseases.
The ability to generate organoids from individuals with specific genetic backgrounds also opens new avenues for personalized medicine. Researchers can use these patient-derived organoids to understand how particular genetic mutations contribute to disease development, enabling the identification of targeted therapeutic strategies.
In cancer research, tumor organoids are particularly valuable, as they retain the genetic and phenotypic characteristics of the original tumors, allowing for the study of tumor heterogeneity and drug resistance. By leveraging organoids, scientists can identify potential biomarkers, screen drugs, and evaluate treatment responses in a way that closely resembles the complexity of human disease, ultimately leading to more effective and personalized therapeutic approaches.
Drug Testing with Organoids
One of the most promising applications of organoids lies in drug testing. Traditional drug testing often relies on two-dimensional cell cultures or animal models, which can yield misleading results due to significant differences in biological responses between these systems and human physiology. Organoids, derived from human tissues, retain the complex architecture and cellular diversity of their organ of origin, allowing researchers to better simulate human responses to drugs. This leads to improved prediction of how potential therapeutics will perform in clinical settings.
One of the major advantages of using organoids in drug testing is their ability to facilitate high-throughput screening of compounds. Researchers can generate large numbers of organoids representing various diseases and patient profiles, enabling the rapid testing of drug libraries to identify effective candidates.
For instance, in cancer research, tumor organoids can be used to evaluate the sensitivity of different cancer types to specific chemotherapeutic agents. By observing how these organoids respond to treatment, researchers can quickly determine which drugs are most effective for particular cancer subtypes, ultimately streamlining the drug development process.
Moreover, organoids offer the potential to minimize the reliance on animal testing, addressing ethical concerns and reducing costs associated with drug development. The use of patient-derived organoids allows for personalized drug testing, where treatments can be tailored to individual patient characteristics.
This not only enhances the likelihood of treatment success but also reduces the risk of adverse effects by allowing for the identification of safe and effective dosages based on the patient’s unique biology. As organoid technology continues to evolve, it is likely to play a crucial role in the future of drug testing, improving the efficiency and reliability of therapeutic development.
Personalized Medicine
Personalized medicine is rapidly transforming the healthcare landscape by enabling treatments that are tailored to the individual characteristics of each patient. Organoids play a pivotal role in this paradigm shift by providing a living model of a patient’s disease. For example, when organoids are derived from a patient’s tumor, they can be used to evaluate the efficacy of different chemotherapy regimens or targeted therapies in real-time.
This capability allows clinicians to identify the most effective treatment options based on the unique genetic and molecular profile of the tumor, ultimately leading to improved outcomes and reduced side effects. Moreover, by using organoids to simulate a patient’s response to various drugs, healthcare providers can make informed decisions, minimizing the trial-and-error approach that often characterizes cancer treatment.
In addition to oncology, organoids have the potential to advance personalized medicine across various medical fields, including rare genetic disorders and infectious diseases. For instance, organoids derived from patients with cystic fibrosis can be used to screen for the best modulators of the defective CFTR protein, offering a tailored therapeutic approach.
Similarly, in infectious diseases, organoids can help researchers understand how different strains of viruses or bacteria interact with human tissues, informing the development of targeted vaccines and treatments. As our understanding of organoid technology deepens, the potential for personalized medicine to enhance patient care will continue to grow, paving the way for more precise, effective, and individualized therapeutic strategies in healthcare.
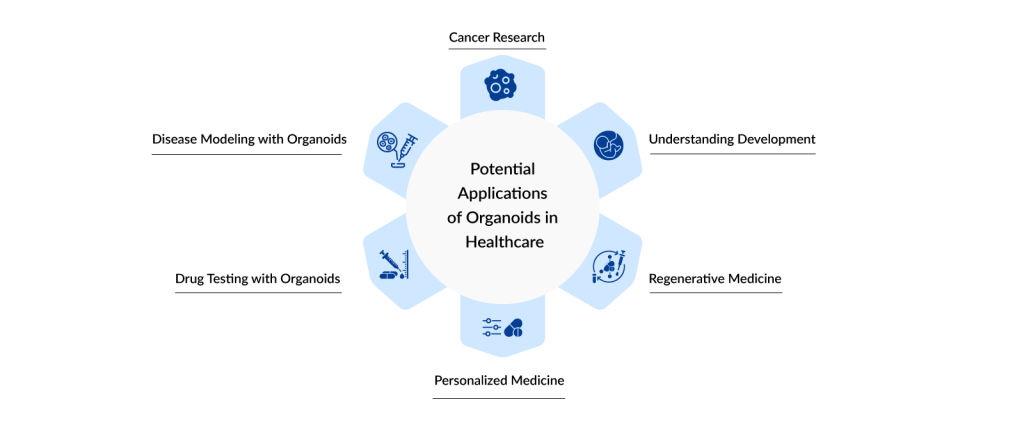
Regenerative Medicine
The potential of organoids in regenerative medicine extends beyond simple tissue repair; they can also be utilized in the development of bioengineered organs. Researchers are exploring methods to scale up organoid cultures to generate larger tissue constructs that could eventually be used for transplantation. For instance, cardiac organoids are being studied for their ability to repair heart tissue following myocardial infarction.
By utilizing patient-derived induced pluripotent stem cells (iPSCs), scientists can create organoids that not only replicate the cellular architecture of the heart but also reflect the genetic background of the patient, thereby reducing the risk of rejection post-transplant. This innovative approach may lead to breakthroughs in treating conditions like heart disease, where organ donation is often limited by availability and compatibility.
Moreover, organoids can serve as powerful tools for studying the mechanisms of tissue regeneration. By examining how organoids respond to injury or stress, researchers can uncover the signaling pathways and cellular behaviors involved in regeneration. This research has implications not only for regenerative medicine but also for understanding diseases characterized by tissue degeneration, such as osteoarthritis or degenerative neurological disorders.
As scientists continue to unravel the complexities of organoid biology, the insights gained will inform the development of therapies that enhance the body’s intrinsic regenerative capabilities, ultimately leading to improved outcomes for patients suffering from chronic conditions and injuries. The ongoing integration of organoid technology into regenerative medicine holds great promise for advancing treatment strategies and enhancing the quality of life for individuals facing a range of health challenges.
Understanding Development
Understanding human development is one of the most profound applications of organoid technology, as it provides insights into the intricate processes that govern organ formation and differentiation. Organoids can recapitulate early embryonic development stages, enabling researchers to study how various cell types interact and contribute to the formation of complex tissues.
For instance, using pluripotent stem cells, scientists have successfully created organoids that resemble various organs, such as the brain, kidney, and intestine. By observing the growth patterns and cellular behaviors within these organoids, researchers can uncover the molecular and genetic underpinnings of normal development and identify the origins of developmental disorders.
Moreover, organoids are instrumental in investigating the effects of genetic mutations on development. For example, researchers have used cerebral organoids to model neurodevelopmental disorders like microcephaly and autism, providing insights into how specific genetic alterations can disrupt normal brain development. This capability allows for a better understanding of the etiology of these conditions and the identification of potential therapeutic targets.
By advancing our knowledge of developmental biology through organoid research, we can improve diagnostic methods, develop targeted interventions, and ultimately enhance outcomes for individuals affected by developmental disorders.
Cancer Research
The role of organoids in cancer research extends beyond simply mimicking tumor biology; they are instrumental in uncovering the mechanisms underlying cancer progression and resistance to therapy. By analyzing how tumor organoids respond to various treatment regimens, researchers can identify critical factors that influence drug sensitivity and resistance.
For instance, through high-throughput drug screening on patient-derived organoids, scientists can determine which therapies are most effective for specific tumor types or even individual patients. This personalized approach can significantly enhance the likelihood of successful outcomes, providing a more targeted treatment strategy that accounts for the unique genetic and molecular characteristics of each patient’s cancer.
Another significant advantage of organoids is their ability to replicate the tumor microenvironment, which plays a critical role in cancer progression and treatment response. Organoids can be co-cultured with stromal cells, immune cells, and extracellular matrix components to create a more realistic representation of the tumor environment.
This setup allows researchers to study the interactions between tumor cells and their microenvironment, including how these interactions contribute to metastasis and immune evasion. By understanding the complexities of these relationships, researchers can develop innovative therapies that target not only the cancer cells but also the supportive cells within the tumor microenvironment, potentially leading to more effective treatment options.
As the field of cancer research continues to evolve, organoid technology is poised to play an even more prominent role in the development of novel therapeutics. Emerging research is focusing on using organoids to study the effects of combination therapies, which are often necessary to overcome drug resistance. By examining the effects of multiple agents on organoid models, researchers can better understand optimal dosing regimens and synergistic effects that could lead to improved treatment protocols.
Furthermore, the integration of organoid technology with genomic and proteomic analyses enables the identification of potential biomarkers that could predict treatment responses, paving the way for more effective precision medicine strategies in oncology. Overall, the use of organoids in cancer research not only enhances our understanding of tumor biology but also accelerates the translation of research findings into clinical applications, ultimately improving patient outcomes.
Conclusion
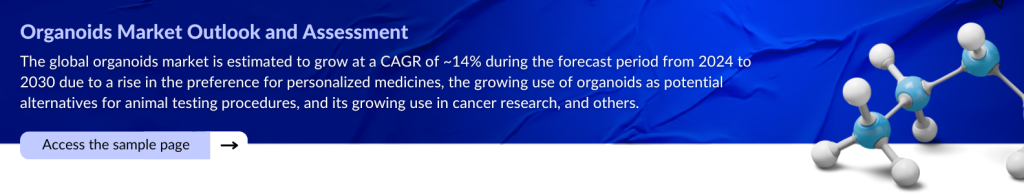
The integration of organoids into healthcare represents a paradigm shift, offering more accurate models for studying human biology and disease. Unlike traditional models, organoids provide a closer approximation of human tissues, enabling researchers to explore disease mechanisms and therapeutic responses with unprecedented precision.
This capability is particularly transformative in personalized medicine, where patient-derived organoids allow for customized treatment plans, reducing trial-and-error approaches and improving patient outcomes. As this technology continues to mature, it promises to shorten the drug development timeline, lower costs, and increase the success rate of new therapies entering the market.
Looking forward, the continued advancement of organoid technology could pave the way for even more revolutionary applications, such as the creation of fully functional organ replacements. As researchers overcome current challenges like scalability, reproducibility, and ethical considerations, the potential for organoids to replace or repair damaged organs becomes increasingly feasible.
Additionally, organoids could serve as a cornerstone for integrative research, combining genomics, bioinformatics, and advanced imaging to deliver comprehensive insights into human health and disease. Ultimately, organoids are not just a tool for research but a harbinger of a more personalized, efficient, and effective era in healthcare.
Downloads
Article in PDF
Recent Articles
- Innovative Pathways in Joint Reconstruction: Market Dynamics and Future Horizons
- Eosolutions Corp’s Dr. Banner Balloon Guide Catheter; US FDA Approves the Cyltezo® Pen; Orlucent’...
- Bridging the gap: Nontuberculous mycobacterium Infections Drug Pipeline
- Cancer-killing virus flees immune destruction and attacks metastatic lung tumors; Urovant’s...
- Non-opioid Analgesics Chronic Pain Treatment: Savior of Underserved Patients