Decoding Parkinson’s Diagnosis with Gene Therapies and Prevention Insights
Dec 31, 2024
Table of Contents
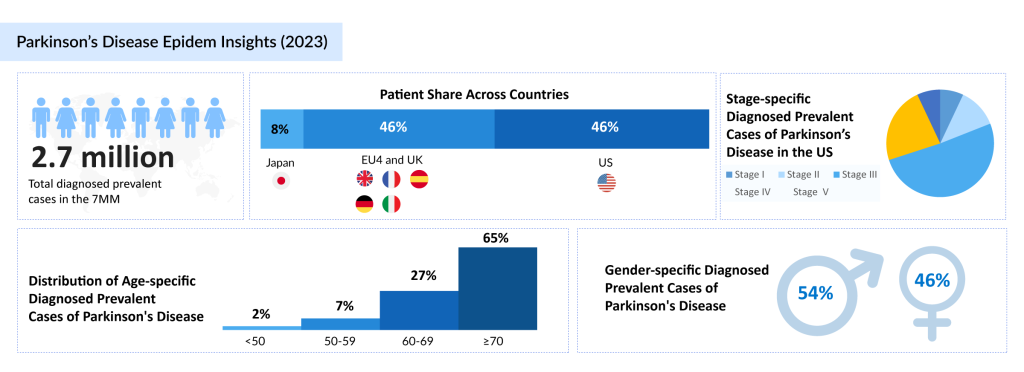
Parkinson’s disease is a progressive neurodegenerative disorder that affects nearly 10 million people worldwide. With the increasing prevalence of Parkinson’s disease due to aging populations and environmental risk factors, this condition profoundly impacts motor functions, cognitive abilities, and overall quality of life. Understanding Parkinson’s disease progression is crucial for implementing effective management strategies.
Early diagnosis is a cornerstone in managing Parkinson’s disease. Detecting the condition during its initial stages can significantly slow down its aggravation, enabling timely interventions such as medication, lifestyle modifications, and therapies that improve patient outcomes. Often, early symptoms are subtle and can include changes in movement, mood, or sleep, making accurate Parkinson’s disease diagnostics essential for effective treatment planning.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- Sobi’s GAMIFANT Approved by FDA as First Treatment for Macrophage Activation Syndrome in Still’s ...
- GE HealthCare’s CARESCAPE Canvas Patient Monitoring Platform; Medtronic’s MiniMed™ 780G Sy...
- Merck to Acquire Harpoon Therapeutics; Novo Nordisk Enters Into Collaborations with Omega Therape...
- Novartis Announces the Positive Results of Phase III NATALEE Trial Evaluating Kisqali; FDA Approv...
- Major Depressive Disorder: Unveiling Market Moves and Commercial Breakthroughs
This article delves into the stages of Parkinson’s disease, examining its progression from mild symptoms to advanced disability. Additionally, it explores the risk factors for Parkinson’s disease, preventive strategies, and groundbreaking innovations in gene therapy. By highlighting the importance of early diagnosis and shedding light on these critical aspects, this resource aims to enhance understanding and foster improved care for individuals living with Parkinson’s disease.
Stages of Parkinson’s Disease and Diagnostic Indicators
Parkinson’s disease is a progressive neurological condition that unfolds in five distinct stages. Understanding these Parkinson’s disease stages helps clinicians and caregivers recognize the trajectory of the disease and implement appropriate interventions. Diagnosing Parkinson’s disease development at each stage involves identifying specific motor and non-motor symptoms, supported by clinical evaluations and advanced diagnostic tools.
Stages of Parkinson’s Disease
- Stage One: Early Parkinson’s Disease
- Symptoms are mild and often localized, such as slight tremors or rigidity on one side of the body.
- Minimal interference with daily activities, making this stage challenging to detect without detailed clinical observation.
- Stage Two: Bilateral Symptoms Appear
- Motor symptoms like tremors, rigidity, and bradykinesia affect both sides of the body.
- Postural changes and difficulties in walking may begin, alongside early non-motor symptoms such as mood changes or fatigue.
- Stage Three: Mid-Stage Parkinson’s Disease
- Loss of balance and slowed movements become more apparent, leading to an increased risk of falls.
- Daily tasks become increasingly difficult without assistance.
- Stage Four: Advanced Parkinson’s Disease
- Severe motor impairments require significant help with daily activities.
- Patients may need mobility aids to navigate, and speech changes often become prominent.
- Stage Five: Late-Stage Parkinson’s Disease
- Patients are typically wheelchair-bound or bedridden.
- Non-motor symptoms like cognitive decline and hallucinations severely impact the quality of life.
Parkinson’s Disease Key Symptoms and Diagnostic Clues at Each Stage
Diagnostic indicators evolve as the disease progresses. In the early stages, subtle motor symptoms like resting tremors and slowed movements are critical diagnostic clues. Non-motor signs such as a reduced sense of smell or sleep disturbances often precede motor symptoms, emphasizing the need for early and comprehensive evaluations.
In the mid to late stages, advanced motor impairments and non-motor symptoms like dysphagia, orthostatic hypotension, and dementia become more apparent. Clinical tools such as the Unified Parkinson’s Disease Rating Scale (UPDRS) and imaging studies like DaTscan help confirm the diagnosis and monitor disease progression.
Challenges in Diagnosing Early-Stage Parkinson’s
Diagnosing early-stage Parkinson’s disease is particularly challenging due to the subtlety and overlap of symptoms with other conditions, such as neurodegenerative disorders. Resting tremors or bradykinesia may initially be misattributed to aging or stress. Early symptoms are often subtle and vary widely among individuals, complicating detection. Non-motor symptoms, such as depression or constipation, are frequently overlooked as they are not immediately associated with Parkinson’s. Moreover, there is no definitive biomarker or diagnostic test, relying instead on clinical evaluations and symptom history, which can lead to misdiagnoses and delays in treatment initiation and care planning.
Innovative diagnostic approaches, including biomarkers and genetic testing, are being developed to address these challenges. Early and accurate Parkinson’s disease diagnostics are vital for implementing treatments that slow Parkinson’s disease development and improve long-term outcomes for patients.
Parkinson’s Disease Risk Factors and Diagnostic Screening
Understanding the risk factors associated with Parkinson’s disease plays a crucial role in early detection and prevention. Both genetic and environmental factors contribute to the onset of Parkinson’s disease, and identifying these risks can help with early Parkinson’s disease diagnostics and monitoring at-risk populations. Advanced diagnostic screening methods are essential in diagnosing Parkinson’s disease early, improving the chances of slowing its deterioration through targeted therapies.
Genetic and Environmental Risk Factors
Genetic risk factors play a significant role in the development of Parkinson’s disease, especially in those with a family history of the condition. Research has identified several genes, such as LRRK2 and SNCA, that are linked to an increased risk of Parkinson’s. Mutations in these genes contribute to the degeneration of neurons that produce dopamine, a hallmark of Parkinson’s disease progression. However, genetic predisposition alone is not sufficient to guarantee the onset of the disease, and other environmental risk factors also play a critical role.
Environmental factors such as exposure to pesticides, toxins, and heavy metals have been associated with an increased risk of developing Parkinson’s disease. Additionally, rural living and certain occupations involving chemical exposure may heighten the risk. Parkinson’s disease is also more common in older adults, with the incidence increasing with age. These combined genetic and environmental factors underscore the importance of Parkinson’s disease diagnostics in identifying individuals who may be at a higher risk for developing the condition.
Advanced Screening Methods for At-Risk Populations
For individuals at high risk of Parkinson’s disease, such as those with a family history or exposure to environmental toxins, advanced screening methods are essential for early diagnosis and intervention. Parkinson’s disease diagnostics have evolved with advancements in imaging technologies, such as DaTscan, which helps evaluate the integrity of dopamine-producing neurons in the brain. Additionally, biomarkers in the blood and cerebrospinal fluid are being researched to detect the early onset of Parkinson’s before significant motor symptoms appear.
Screening for Parkinson’s disease in at-risk populations can also include the use of neurophysiological tests to assess motor function and changes in brain activity. Early intervention through advanced screening methods enables more effective treatment options to slow the progression of Parkinson’s disease, especially in its early stages. Furthermore, genetic testing for mutations linked to Parkinson’s can help identify individuals who may benefit from closer monitoring and personalized treatment strategies to prevent or delay the disease’s onset.
Parkinson’s Disease Diagnostic Tools and Techniques
The accurate and early diagnosis of Parkinson’s disease is crucial for optimizing treatment outcomes and improving the quality of life for patients. Recent advancements in neuroimaging technologies and diagnostic tools have revolutionized the approach to Parkinson’s disease diagnostics. Techniques such as MRI, PET scans, and DaTscan, along with clinical evaluations, allow healthcare professionals to identify the disease at its earliest stages and accurately monitor its progression. The development of innovative diagnostic devices, such as QuantalX’s Delphi-MD and Sunbird Bio’s blood test, further contributes to the personalization and precision of Parkinson’s disease diagnostics, offering hope for faster and more accurate diagnoses.
Neuroimaging Technologies (MRI, PET, and DaTscan)
Neuroimaging technologies like MRI (Magnetic Resonance Imaging), PET (Positron Emission Tomography), and DaTscan are integral in diagnosing Parkinson’s disease by providing detailed images of brain structure and activity. MRI helps to rule out other potential causes of the symptoms, like strokes or tumors, by creating high-resolution images of the brain. PET scans, on the other hand, detect changes in brain function by measuring the activity of specific areas, such as the dopaminergic system, which is often impaired in Parkinson’s disease. DaTscan is particularly useful for identifying dopamine transporter dysfunction, a hallmark of Parkinson’s, by providing a clear visualization of dopamine transporters in the brain, which are typically reduced in individuals with the disease.
In October 2024, QuantalX Neuroscience announced a breakthrough in Parkinson’s disease diagnostics with its Delphi-MD device, which is enhancing personalized management and improving early detection of Parkinson’s disease. This innovative technology offers a new method for identifying Parkinson’s disease and subtyping it early, paving the way for more effective treatments. By enabling precise diagnostics and reducing delays in treatment, the Delphi-MD device supports quicker interventions, benefiting patients, healthcare systems, and pharmaceutical companies alike.
Clinical Assessment and Motor Symptom Evaluation
In addition to advanced imaging technologies, clinical assessment, and motor symptom evaluation remain fundamental in diagnosing Parkinson’s disease. Motor symptoms such as tremors, rigidity, bradykinesia, and postural instability are often the first signs of Parkinson’s disease growth. A comprehensive clinical assessment involves evaluating these motor symptoms, as well as assessing the patient’s response to various physical tasks, which can provide significant insight into the severity of the disease. The Unified Parkinson’s Disease Rating Scale (UPDRS) is often used by clinicians to measure the severity of motor symptoms and track disease progression.
Recent advancements in Parkinson’s disease diagnostics have led to the development of more objective evaluation tools, like the Delphi-MD device from QuantalX Neuroscience. By offering precise, real-time analysis of motor functions, these tools allow for more accurate diagnoses and more tailored treatment plans for Parkinson’s patients. This development not only aids in early detection but also improves the management of the disease, allowing clinicians to track the effects of therapeutic interventions more effectively.
Non-Motor Symptoms as Diagnostic Red Flags
While motor symptoms are the most commonly recognized indicators of Parkinson’s disease, non-motor symptoms often appear early in the disease and can serve as critical diagnostic red flags. Symptoms such as depression, cognitive impairment, sleep disturbances, and autonomic dysfunction may manifest before motor symptoms and can often go unnoticed or be mistaken for other conditions. Parkinson’s disease diagnostics must therefore consider these non-motor symptoms as part of the diagnostic process, particularly when patients exhibit early signs of cognitive decline or mood disorders.
The ability to detect these non-motor symptoms early can provide invaluable information for a comprehensive diagnosis. For example, Sunbird Bio’s technology, which detects aggregated alpha-synuclein proteins in blood samples, demonstrates significant potential in diagnosing Parkinson’s disease with 86% accuracy. These proteins are thought to be involved in the disease’s pathogenesis and could be present even in the early stages of Parkinson’s disease. This type of innovative diagnostic tool, combined with clinical evaluation and imaging technologies, may greatly improve early diagnosis, leading to more effective treatment and better patient outcomes.
Emerging Biomarkers in Parkinson’s Disease Diagnosis
Advancements in Parkinson’s disease diagnosis have led to the identification of several emerging biomarkers, which promise to revolutionize how the disease is detected and monitored. As the Parkinson’s disease treatment landscape continues to evolve, research into biomarkers plays a critical role in early diagnosis, improving treatment strategies, and facilitating the development of Parkinson’s disease emerging drugs. Emerging biomarkers are offering new insights into the pathophysiology of the disease, enabling more personalized treatments and early interventions that could significantly alter the course of Parkinson’s disease progression.

Alpha-Synuclein Detection
One of the most promising Parkinson’s disease emerging biomarkers is alpha-synuclein, a protein that plays a key role in the development of Parkinson’s disease. Abnormal aggregation of alpha-synuclein in the brain is a hallmark of the disease, contributing to the death of dopamine-producing neurons and the characteristic motor and non-motor symptoms of Parkinson’s. Advances in detecting aggregated alpha-synuclein in blood and cerebrospinal fluid (CSF) have made it possible to diagnose Parkinson’s disease earlier, even before the onset of motor symptoms.
For instance, in November 2024, Sunbird Bio released data showing that its diagnostic technology could successfully detect aggregated alpha-synuclein proteins in blood samples from Parkinson’s disease patients with 86% accuracy. This breakthrough provides an objective and non-invasive method for identifying Parkinson’s disease at earlier stages, offering clinicians a valuable tool to distinguish it from other neurodegenerative conditions. The detection of alpha-synuclein in blood and CSF could soon become a standard practice in Parkinson’s disease diagnosis, leading to more effective and timely interventions in the future.
Role of Blood and Cerebrospinal Fluid (CSF) Biomarkers
Blood and cerebrospinal fluid (CSF) biomarkers are playing an increasingly important role in Parkinson’s disease diagnosis. Traditionally, Parkinson’s disease has been diagnosed based on clinical symptoms and motor evaluations. Still, with the rise of biomarker research, doctors can now gain a more accurate understanding of the disease’s progression and potentially detect it earlier.
CSF is often considered a more direct reflection of brain health, making it an important source for identifying biomarkers like alpha-synuclein, tau, and other proteins associated with neurodegenerative diseases. Blood biomarkers, on the other hand, are less invasive and offer the advantage of being more easily accessible for regular monitoring. Both blood and CSF biomarkers are essential in identifying Parkinson’s disease advancement and helping track the effectiveness of new Parkinson’s disease emerging drugs. Biomarker analysis of these fluids is quickly becoming a critical aspect of clinical trials and is likely to play a significant role in improving the precision of treatments for Parkinson’s disease.
Breakthroughs in Biomarker Research
There have been several breakthroughs in Parkinson’s disease biomarker research in recent years, offering new hope for patients and healthcare providers alike. Along with the advancements in alpha-synuclein detection, researchers are exploring other potential biomarkers that could reveal more about the early stages of the disease and provide insights into its molecular mechanisms. New studies focus on genetic biomarkers, inflammatory markers, and biomarkers related to neuronal damage that could offer even greater precision in Parkinson’s disease diagnosis.
These breakthroughs are not only improving early detection but are also facilitating the development of new Parkinson’s disease emerging drugs. By identifying biomarkers that can be used to track disease progression, researchers can better understand how therapies work and predict their effectiveness. This will allow pharmaceutical companies to create more targeted treatments for Parkinson’s patients, potentially slowing or halting the disease’s escalation. As the Parkinson’s disease market continues to grow, the identification of these emerging biomarkers will be pivotal in shaping the future of Parkinson’s disease care and ensuring better outcomes for patients.
Gene Therapy as a Diagnostic and Therapeutic Tool
Gene therapy For Parkinson’s Disease is emerging as a promising diagnostic and therapeutic tool in the management of the disease, offering the potential to address both the genetic underpinnings of the disease and its clinical manifestations. With the growing understanding of genetic contributions to Parkinson’s disease, advancements in genetic testing are enhancing Parkinson’s disease diagnosis and facilitating early detection. As research into Parkinson’s disease emerging drugs continues to progress, gene therapy could play a pivotal role in not only diagnosing the condition but also offering targeted, personalized treatments.
Genetic Testing for Parkinson’s Risk Assessment
Genetic testing is becoming increasingly important in the Parkinson’s disease treatment market for risk assessment and early diagnosis. By identifying these genetic variations through advanced testing, healthcare providers can more accurately assess an individual’s risk of developing Parkinson’s, even before clinical symptoms appear.
With the rise of genetic testing for Parkinson’s disease risk, clinicians are able to better inform patients about their likelihood of developing the disease, allowing for proactive monitoring and intervention. Additionally, genetic testing aids in identifying familial forms of Parkinson’s disease, where inheritance patterns play a crucial role in diagnosis.
As part of Parkinson’s disease diagnostics, this testing could lead to earlier, more personalized care plans, optimizing therapeutic outcomes and potentially slowing disease intensifying.
Advances in Gene Therapy Targeting Parkinson’s Pathology
Recent breakthroughs in gene therapy offer exciting prospects for Parkinson’s disease treatment by targeting the underlying pathology of the disease at a molecular level. Advances in gene therapy targeting Parkinson’s pathology aim to correct or mitigate the genetic factors that contribute to the degeneration of dopamine-producing neurons in the brain. By delivering genes that encode for proteins involved in neuron survival or the synthesis of dopamine, these therapies have the potential to slow or even reverse some of the symptoms of Parkinson’s disease.
One promising approach involves the use of viral vectors to deliver genes that either restore dopamine production or protect neurons from further damage. In preclinical and early-stage clinical trials, gene therapy has shown potential in improving motor symptoms and overall quality of life for patients with Parkinson’s disease. As research progresses, gene therapy may not only serve as a therapeutic tool to address the root causes of Parkinson’s but also as a diagnostic tool, helping to pinpoint specific genetic factors that influence disease progression. These developments are poised to redefine the landscape of Parkinson’s disease emerging drugs and open new avenues for targeted therapies that address both genetic and environmental factors contributing to the disease.
Prevention Through Early Detection
Early detection of Parkinson’s disease is key to preventing or delaying the growth of symptoms. Identifying the disease at its early stages allows for targeted interventions, such as lifestyle modifications, that may help slow disease progression. Early diagnosis allows healthcare providers to recommend personalized strategies, including exercise, diet adjustments, and stress management, to enhance brain health and improve long-term outcomes.
With early detection, patients can adopt lifestyle modifications to slow Parkinson’s disease progression. Physical activity, dietary changes, and cognitive exercises can support motor function and reduce inflammation, potentially delaying the onset of more severe symptoms. These interventions, when applied early, can significantly improve the quality of life for individuals with early Parkinson’s disease.
Monitoring preclinical symptoms, such as subtle tremors or changes in sleep patterns, is crucial for early intervention. Identifying and managing these symptoms allows healthcare providers to implement timely treatments, reducing the risk of severe development. By monitoring motor and non-motor symptoms, healthcare professionals can offer proactive care, improving the overall outcome for at-risk patients.
Future of Parkinson’s Disease Diagnostics
Parkinson’s disease remains a major global health challenge, affecting millions and significantly impacting patients’ quality of life. Understanding Parkinson’s disease advancement, from its early stages to advanced disability, is essential for effective management and intervention. Early detection is critical in slowing the disease, allowing for timely treatments that improve patient outcomes. Innovations in Parkinson’s disease diagnostics, including neuroimaging technologies, emerging biomarkers, and gene therapy, pave the way for more precise and personalized care.
By focusing on early Parkinson’s disease diagnostics, lifestyle modifications, and advancements in gene therapy and biomarker research, healthcare providers can offer proactive management strategies that delay the onset of more severe symptoms. With ongoing research into genetic risk factors and novel therapeutic approaches, the future of Parkinson’s disease care holds great promise. As the Parkinson’s disease therapeutic market continues to evolve, early detection and intervention will be pivotal in improving the lives of those affected, offering hope for better outcomes in the years to come.
Downloads
Article in PDF
Recent Articles
- Prosecutors rope Pfizer; Pharma groups to FDA; Regeneron simulates; Otsuka & Lundbeck revive...
- Cambrex acquires Avista; Sobi pays $50M; LEO Pharma signs deal; Boston Scientific remunerates
- BeiGene’s BRUKINSA Gets FDA Accelerated Approval; GSK’s Positive Results in DREAMM-8 ...
- Boston Scientific INGEVITY™ gets Expanded Indication and acquires Silk Road Medical; FDA Approves...
- Notizia