Helicobacter pylori Infections Treatment: Emerging Molecular Targets
Sep 09, 2024
Table of Contents
Helicobacter pylori infection is among the most widespread chronic bacterial infections globally, affecting roughly half of the world’s population. H. pylori is classified as a Class I carcinogen by the WHO and is recognized as a qualifying pathogen under the US FDA’s GAIN Act. It is the most significant known risk factor for noncardia gastric adenocarcinoma and is typically linked with chronic gastritis, the formation of preneoplastic lesions, or peptic ulcer disease.
It is usually contracted in childhood and is a major risk factor for non-cardia gastric adenocarcinoma, the most common type of stomach cancer, as well as peptic ulcer disease. According to DelveInsight’s estimates, the diagnosed prevalent cases of H. pylori infection in the 7MM were found to be approximately 323 million cases in 2023. These cases are projected to increase during the forecast period (2024–2034).
Downloads
Article in PDF
According to estimates based on DelveInsight’s epidemiology model for age-specific H. pylori infection cases, in the 7MM, the above 40 age group accounted for the majority, with nearly 60% of the H. pylori infection, in 2023.
The existing treatment approach for H. pylori infection focuses on therapy rather than prevention. The primary objective is to eliminate the bacteria, which is crucial for healing peptic ulcers and avoiding recurrences. However, increasing antibiotic resistance has turned this into a worldwide problem.
The Role of PPIs in Treating H. pylori Infections
The primary treatment for H. pylori infections involves Proton Pump Inhibitors (PPIs), which are medications that dramatically lower stomach acid production. This reduction in acidity makes it harder for the bacteria to thrive. Common PPIs include omeprazole, lansoprazole, pantoprazole, rabeprazole, and esomeprazole.
However, PPIs alone aren’t sufficient to eliminate H. pylori. Doctors usually recommend a combined approach that includes both antibiotics and a PPI. The choice of antibiotics depends on factors such as local resistance patterns and the patient’s health history. Frequently used antibiotics for treating H. pylori are clarithromycin, amoxicillin, metronidazole, rifabutin, and tetracycline. Each antibiotic targets the bacteria differently, which helps prevent the development of resistance.
Antibacterial drugs such as clarithromycin, amoxicillin, metronidazole, and tetracycline play a crucial role in the treatment of Helicobacter pylori infections. Clarithromycin works by binding to the 50S ribosomal subunit, blocking bacterial protein synthesis. Amoxicillin interferes with cell wall formation by inhibiting transpeptidase enzymes. Metronidazole is activated within the cell, causing damage to bacterial DNA and hindering nucleic acid synthesis. Tetracycline inhibits protein synthesis by attaching to the 30S ribosomal subunit. Together, these antibiotics effectively target and inhibit H. pylori growth and replication.
Antisecretory drugs, particularly proton pump inhibitors (PPIs) like omeprazole and lansoprazole, enhance the effectiveness of antibacterial therapy by permanently blocking the H+/K+-ATPase proton pump on gastric parietal cells, which decreases stomach acid production. Reduced gastric acidity improves the efficacy of antibiotics against H. pylori and aids in healing gastrointestinal mucosal damage, such as peptic ulcers and gastritis, by minimizing acid-induced tissue injury and inflammation. Combining antibacterial and antisecretory medications maximizes bacterial eradication and ulcer healing, leading to improved treatment outcomes for H. pylori infections.
TALICIA (RHB-105), marketed by RedHill Biopharma, is a single oral capsule combining omeprazole (a PPI), amoxicillin (a penicillin-type antibiotic), and rifabutin (a rifamycin antibiotic) for treating H. pylori infections in adults. Omeprazole reduces stomach acid, creating a more effective environment for the antibiotics. Amoxicillin disrupts bacterial cell walls, causing cell death, while rifabutin prevents bacterial RNA synthesis. This combination therapy addresses bacterial growth, reduces stomach acidity, and combats antibiotic resistance, offering an effective treatment for H. pylori infections.
Potassium-Competitive Acid Blockers: A New Approach for H. pylori Infections Treatment
Potassium-competitive acid blockers (P-CABs) function by competitively blocking potassium ions from binding to the H+, K+ ATPase enzyme in gastric parietal cells, which interferes with the final stage of gastric acid secretion. This mechanism is distinct from that of conventional proton pump inhibitors (PPIs), potentially providing a stronger and longer-lasting suppression of acid production.
FDA has approved 2 therapies from the P-CABs class namely, VOQUEZNA TRIPLE PAK and VOQUEZNA DUAL PAK (Phathom Pharmaceuticals) and TAKECAB (Takeda Pharmaceutical/Otsuka Pharmaceutical).
Vonoprazan is an oral potassium-competitive acid blocker (PCAB) that is packaged with antibiotics. PCABs represent a new class of medications designed to inhibit stomach acid secretion. Vonoprazan can offer acid suppression that achieves pH levels necessary to boost antibiotic effectiveness. In October 2023, the US FDA approved the reformulated vonoprazan tablets for use in VOQUEZNA TRIPLE PAK (vonoprazan, amoxicillin, clarithromycin) and VOQUEZNA DUAL PAK (vonoprazan, amoxicillin) for treating H. pylori infections in adults. Both VOQUEZNA TRIPLE PAK and VOQUEZNA DUAL PAK, developed by Phathom Pharmaceuticals, were approved by the US FDA in May 2022 for the same indication.
TAKECAB or TAK-438, developed by Takeda, is an innovative antisecretory medication designed for treating acid-related disorders. It features a unique mechanism known as potassium-competitive acid blockers (P-CABs), which inhibit the binding of potassium ions to H+, K+ ATPase during the final stage of gastric acid secretion in parietal cells. TAKECAB offers potent and long-lasting inhibition of acid secretion. Takeda is partnering with Otsuka Pharmaceuticals to promote TAKECAB.
Apart from PPIs and P-CABs, the US FDA has approved various combination therapies, including NEXIUM and PREVPAC, and AbbVie’s PYLERA, all of which are now available in generic versions. Although antibiotic resistance rates have increased in the last decade and reduced the efficacy of recommended treatments. However, due to the guideline update and designation, the H pylori treatment landscape has also seen many FDA approvals.
Emerging Options for H. pylori Infections Treatment
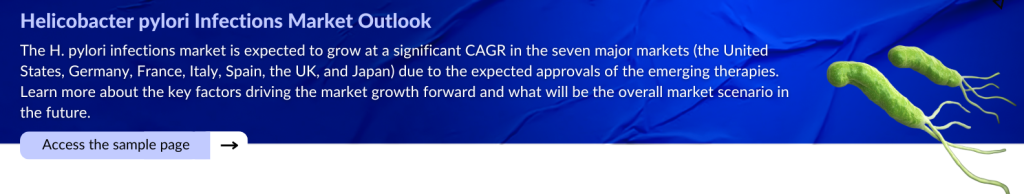
Given the limited development of new therapies for H. pylori, with few novel mid or late-stage treatments and most trials focusing on enhancing existing combinations, the market for H. pylori is expected to experience some shifts.
The late-stage H. pylori pipeline is limited and certain therapies are being developed by Nexbiome Therapeutics, among others. H. pylori therapies are also being developed by TrioMedicine, and TenNor Therapeutics, among others.
Nexbiome Therapeutics’ BGA-1901
BGA-1901 is in development to address H. pylori infections. It is a single-strain live biotherapeutic featuring lactobacillus casei rhamnosus LCR35 and is being designed as a microbiome-based treatment. The drug is presently undergoing Phase III clinical trials.
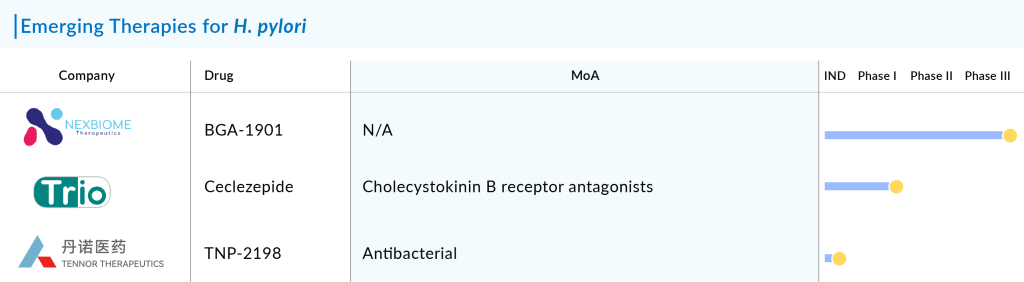
Trio Medicines’ Ceclazepide (TR2-A)
Ceclazepide, developed by Trio Medicines, is a prodrug and a new, powerful, and highly specific antagonist for the gastrin/CCK2 receptor. It is currently undergoing Phase I clinical trials for treating H. pylori infection.
TenNor Therapeutics’ Rifasutenizole (TNP-2198)
Rifasutenizole (TNP-2198) is a distinctive multitarget drug conjugate that combines synergistic actions to provide strong bactericidal effects against drug-resistant H. pylori strains while maintaining a very low rate of spontaneous resistance. It has a broad range of uses, including treating H. pylori infections, bacterial vaginosis, and Clostridium difficile infections.
Supported by China’s National Major New Drug Innovation grant, TNP-2198 has received IND approval and QIDP designation from the US FDA for H. pylori infection treatment. The company has completed five clinical trials in China and is now conducting a multi-center, randomized, double-blind Phase III trial of bismuth-containing quadruple therapy to support its New Drug Application in both China and the US. This Phase III trial aims to develop an effective, safe, and simplified eradication regimen compatible with urea breath tests (UBT), with the potential to implement large-scale H. pylori screening and eradication strategies to help prevent gastric cancer in high-risk populations. Additionally, TNP-2198 is undergoing a Phase II trial for Clostridioides difficile infection and bacterial vaginosis.
The anticipated launch of these emerging therapies for H. pylori are poised to transform the market landscape in the coming years. As these cutting-edge therapies continue to mature and gain regulatory approval, they are expected to reshape the H. pylori treatment market landscape, offering new standards of care and unlocking opportunities for medical innovation and economic growth.
The Evolving Landscape of H. pylori Infections Treatment
Most H. pylori infection treatment guidelines suggest using triple therapies—combinations of antibiotics with either antisecretory agents, PPIs, or other acid-regulating drugs—as the primary approach for eradicating H. pylori. Single-drug therapies are ineffective because stomach acidity diminishes the effectiveness of antibiotics. Additionally, growing antibiotic resistance complicates treatment, with only a few antibiotics like clarithromycin, amoxicillin, metronidazole, fluoroquinolones (such as levofloxacin and norfloxacin), tetracycline, and rifabutin remaining effective against H. pylori.
Current guidelines emphasize that H. pylori eradication therapy should be selected based on the regional prevalence of clarithromycin resistance and local conditions, as these factors significantly impact treatment efficacy. There is variation in approved therapies by region, with different therapies being authorized at different times in various countries.
RedHill Biopharma’s TALICIA, a rifabutin-based therapy, is commonly used as a second-line treatment. With 8 years of market exclusivity, it could be transformative for patients with resistance to clarithromycin and metronidazole.
Phathom Pharmaceuticals’ P-CAB combination, including VOQUEZNA, is another noteworthy drug. Approved by the US FDA in 2022 and recently reformulated and reintroduced in the US in 2023, it is available in both triple and dual packs.
As per DelveInsight, the total market size of Helicobacter pylori infection in the 7MM was USD 2.6 million in 2022 and is projected to increase during the forecast period (2023–2034). According to DelveInsight’s analysis, the H. pylori infection market size is expected to grow due to the recent approval of combination therapies, propelled by increasing disease prevalence and changing treatment paradigms in the coming years.
However, the rise of antibiotic resistance has prompted a shift towards more tailored approaches. Newer strategies include the use of alternative antibiotics, bismuth-based quadruple therapy, and individualized treatment plans based on resistance profiles. Additionally, emerging research into vaccines and novel therapeutic agents offers promising avenues for more effective and less disruptive treatment options. As our knowledge of H. pylori continues to grow, personalized and adaptive treatment strategies are becoming central to improving patient outcomes and managing this persistent infection.
Downloads
Article in PDF