Mucopolysaccharidosis: How the Different Types Affect Patients and Treatment Approaches?
Mar 19, 2025
Table of Contents
Mucopolysaccharidosis (MPS) is a group of rare genetic disorders affecting roughly 1 in 25,000 births, yet its impact is profound. Caused by enzyme deficiencies, MPS leads to the buildup of complex sugars in cells, resulting in progressive damage to the heart, bones, brain, and other organs. Symptoms can vary widely — from stunted growth and joint stiffness to vision and hearing loss. While there’s no cure yet, enzyme replacement therapies and other mucopolysaccharidosis treatments can help manage symptoms and improve quality of life. Raising awareness is crucial — early diagnosis can make all the difference in the fight against MPS.
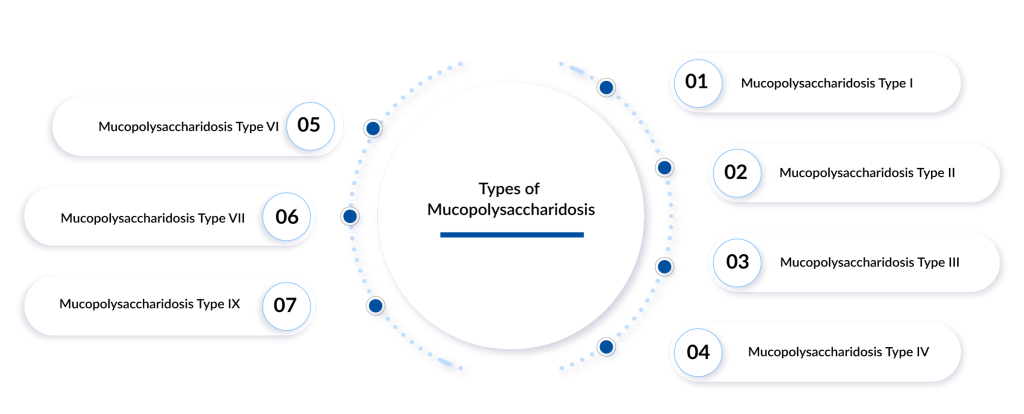
Types of Mucopolysaccharidosis
There are seven primary types of MPS, each resulting from a deficiency in specific lysosomal enzymes involved in GAG breakdown. Let’s delve into each type of mucopolysaccharidosis in detail.
Downloads
Article in PDF
Recent Articles
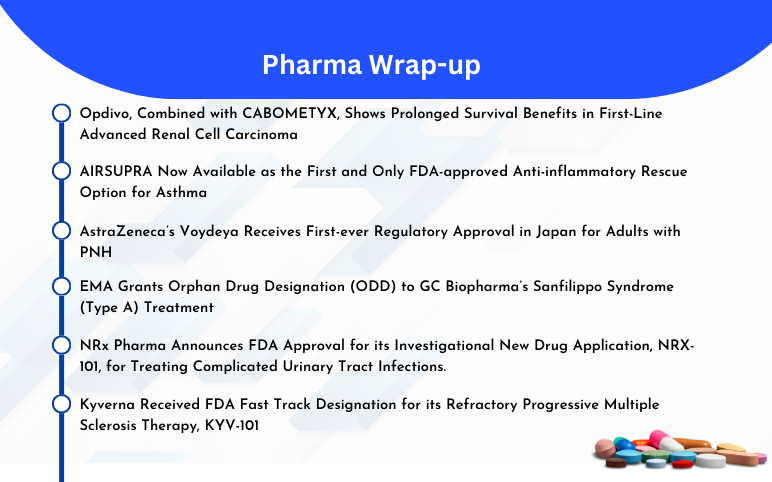
- CTEXLI Approved for Cerebrotendinous Xanthomatosis; SIGX1094 Wins Fast Track for Diffuse Gastric ...
- Rising of Orphan Drug Development
- Mucopolysaccharidosis I (MPS I) (Hurler Syndrome) – a lesser developed window
- BMS, and Exelixis’s Opdivo + CABOMETYX in First-Line Advanced Renal Cell Carcinoma; AIRSUPRA Now ...
- Hunter Syndrome Market experiences a positive push as the pharma companies spot the untapped oppo...
Mucopolysaccharidosis Type I
MPS I is a rare, inherited lysosomal storage disorder caused by a deficiency in the enzyme alpha-L-iduronidase (IDUA), essential for breaking down glycosaminoglycans (GAGs) like dermatan sulfate and heparan sulfate. Without sufficient IDUA, these substances accumulate, causing progressive cellular and tissue dysfunction that affects multiple organ systems, including the skeletal, cardiovascular, respiratory, and nervous systems.
MPS I presents as a clinical spectrum, ranging from severe Hurler syndrome to milder Scheie syndrome. In 2024, DelveInsight estimated approximately 660 diagnosed prevalent cases of MPS I across the 7MM, as per DelveInsight. The United States accounted for 36% of these cases, EU4 and the UK made up nearly 60%, and Japan represented 4%.
Treatment strategies vary based on disease severity. Hematopoietic stem cell transplantation (HSCT) is the standard of care for severe MPS I (MPS IH), particularly in children under two, and is occasionally used for attenuated forms. HSCT allows donor-derived cells to produce IDUA, cross the blood-brain barrier, and reduce CNS involvement. While HSCT slows disease progression, preserves cognitive function, and improves survival, its impact on skeletal abnormalities is limited, and the procedure carries significant risks.
Enzyme replacement therapy (ERT) with laronidase addresses non-CNS symptoms, improving hepatosplenomegaly, respiratory function, mobility, and joint flexibility. ERT is most effective when initiated early, although immune responses may reduce its long-term efficacy. Combining short-term ERT with HSCT is an emerging approach, stabilizing patients before transplant, reducing GAG accumulation, and improving engraftment success for better long-term outcomes.
Currently, ALDURAZYME (laronidase) is the only approved ERT for MPS I. Developed by BioMarin Pharmaceutical and Genzyme (Sanofi), this recombinant glycoprotein helps reduce systemic disease burden by breaking down GAGs. ALDURAZYME was approved in the U.S. in April 2003, followed by approvals in the EU4, the UK (June 2003), and Japan (2006). Although its patent has expired, no biosimilars or alternative biologics have been approved, underscoring the urgent need for new treatment options.
Emerging therapies include OTL-203, Lepunafusp alfa (JR-171), and RGX-111. OTL-203, developed by Orchard Therapeutics and Kyowa Kirin, it is a HSC gene therapy. Administered via IV infusion, it is currently in Phase III clinical trials for the treatment of MPS IH. The anticipated application timeline is 2028, with potential US approval in 2029, assuming priority review.
Lepunafusp alfa (JR-171), developed by JCR Pharmaceuticals, is an ERT (Iduronidase replacement) administered via IV infusion. It is currently in Phase I/II clinical trials for the treatment of MPS IH. RGX-111, developed by REGENXBIO and Nippon Shinyaku, is an IDUA Gene Delivery. It is currently in Phase I/II clinical trials for the treatment of MPS I.
Despite available treatments, there remains a significant need for improved therapies with better efficacy, reduced risks, and enhanced CNS benefits to address the unmet medical needs in MPS I care. According to DelveInsight’s analysis, the MPS I market in the 7MM was valued at approximately USD 145 million in 2024. Over the forecast period from 2025 to 2034, this market is projected to grow at a CAGR of 8.0%. This growth is mainly attributed to the launch of emerging therapies in the coming years.
Mucopolysaccharidosis Type II (Hunter Syndrome)
Hunter syndrome is a rare X-linked recessive disorder for which several initiatives are focused on improving early diagnosis and timely treatment. Its low prevalence makes identifying affected individuals within large populations difficult. Organizations such as the MPS Society, Genes In Life, Angel’s Hand Foundation, and The Global Genes Project are working to enhance the quality of life for patients and their families.
According to DelveInsight’s analysis, there were 1,190 diagnosed prevalent cases of Hunter syndrome in the 7MM in 2023, with cases expected to rise over the forecast period. In the US, nearly 65% of cases were classified as severe in 2023.
Current treatment options for Hunter syndrome include enzyme replacement therapy (ERT), hematopoietic stem cell transplantation (HSCT), and bone marrow transplantation (BMT). Approved therapies include — ELAPRASE (Takeda), HUNTERASE (GC Pharma), and IZCARGO (JCR Pharmaceuticals).
Emerging therapies such as DNL310 (Denali Therapeutics) and RGX-121 (REGENXBIO) are being developed to provide safer and more effective treatment options. The MPS II treatment landscape is expected to see significant advancements between 2024 and 2034 with the introduction of these innovative therapies currently in clinical development.
Mucopolysaccharidosis Type III (Sanfilippo Syndrome)
Mucopolysaccharidosis III (MPS III), or Sanfilippo syndrome, is a rare genetic disorder that causes severe and progressive brain damage, classifying it as a form of childhood dementia. It stems from a deficiency in an enzyme needed to break down and recycle heparan sulfate, a complex sugar molecule. The buildup of heparan sulfate in cells, especially in the central nervous system, leads to cognitive decline and neurological impairment.
MPS III is divided into four subtypes—A, B, C, and D—each caused by mutations in different genes. While all subtypes result in cognitive decline, the severity and rate of progression vary depending on the specific genetic mutation.
Currently, there are no approved treatments for MPS III. Enzyme replacement therapy (ERT) has not shown effectiveness, and bone marrow transplants have had poor outcomes. Research is now focused on gene therapy, chaperone therapy, and intrathecal enzyme therapy as potential solutions.
Several biopharma companies, including Allievex, Denali Therapeutics, Orchard Therapeutics, Sobi, and Ultragenyx, among others, are working on novel MPS III treatments. Promising drug candidates that could significantly impact the forecast period include AX 250, DNL126, UX111 (rebisufligene etisparvovec), OTL-201, and others.
In June 2024, Denali Therapeutics announced that the FDA had selected DNL126 for participation in the Support for Clinical Trials Advancing Rare Disease Therapeutics (START) Pilot Program. DNL126 is an investigational enzyme replacement therapy designed to cross the BBB for the potential treatment of MPS IIIA (Sanfilippo syndrome type A).
Gene therapy holds significant promise for MPS III, as correcting the underlying genetic defect could lead to meaningful improvements in patient outcomes. Ongoing research and innovative approaches are expected to drive the MPS III market forward, creating new opportunities for effective treatments and improving the outlook for patients with this devastating condition.
Mucopolysaccharidosis Type IV (Morquio Syndrome)
Mucopolysaccharidosis IV (MPS IV), or Morquio syndrome, is a rare autosomal recessive lysosomal storage disorder caused by a deficiency in specific enzymes involved in breaking down glycosaminoglycans (GAGs). This enzymatic deficiency leads to GAG accumulation in tissues, causing progressive skeletal abnormalities, restricted growth, and other systemic complications. However, cognitive function typically remains unaffected in individuals with MPS IV.
Symptoms usually appear between ages 1 and 3, with growth slowing and often stopping around age 8. In severe cases (MPS IVA), life expectancy is significantly reduced, with many patients not surviving beyond their 20s or 30s.
The global prevalence of Morquio syndrome is low, with an estimated point prevalence of approximately 1 per 599,000 in the United Kingdom. The rarity of the disease presents challenges in diagnosis, raising awareness, and developing targeted therapies.
Current treatment strategies for MPS IV primarily focus on managing symptoms and improving quality of life. ERT has been a cornerstone of treatment, aiming to supplement the deficient enzyme and reduce GAG accumulation. However, ERT is often associated with high costs and may not be accessible to all patients, especially in developing countries. Supportive care, including surgical interventions to address skeletal abnormalities and respiratory issues, plays a crucial role in the comprehensive management of the disease.
The MPS IV treatment market is expanding due to increased R&D activity and a growing focus on innovative therapeutic approaches. Advancements in gene therapy, improved diagnostic methods, and greater advocacy efforts are driving market growth, enhancing patient outcomes, and improving access to treatments.
Mucopolysaccharidosis Type VI (Maroteaux-Lamy Syndrome)
Mucopolysaccharidosis VI (MPS VI), also known as Maroteaux-Lamy syndrome, is a rare lysosomal storage disorder caused by a deficiency of the enzyme arylsulfatase B (ARSB). This enzyme is responsible for breaking down GAGs, specifically dermatan sulfate.
The global prevalence of MPS VI is estimated to be between 1 in 250,000 to 1 in 600,000 live births. The disease exhibits variability in severity, with a higher incidence reported in certain populations, such as in Brazil and Turkey. Due to its rarity and the wide spectrum of disease presentation, diagnosis is often delayed, contributing to disease progression before treatment can be initiated.
Currently, enzyme replacement therapy (ERT) with galsulfase (NAGLAZYME), approved by the FDA in 2005, remains the standard of care. Galsulfase helps reduce the accumulation of dermatan sulfate and alleviates some symptoms, but it requires lifelong weekly infusions and does not effectively address all systemic complications, such as skeletal and cardiac issues. Symptomatic management, including orthopedic surgery, respiratory support, and physical therapy, is often required alongside ERT.
Emerging therapies for MPS VI aim to overcome the limitations of ERT. Gene therapy is showing promise, with approaches designed to deliver a functional copy of the ARSB gene, enabling long-term endogenous production of the enzyme. Substrate reduction therapy (SRT) and chaperone therapy are also under investigation, targeting the underlying disease mechanism at the molecular level.
Hematopoietic stem cell transplantation (HSCT) has been explored in severe cases, with some success in reducing GAG accumulation, but its use is limited by procedural risks and the availability of suitable donors. Clinical trials are currently underway to assess the efficacy and safety of novel gene-editing techniques and next-generation ERT with improved biodistribution and reduced immunogenicity.
The MPS VI market is expected to grow steadily due to increasing awareness, improved diagnostic capabilities, and the development of novel therapies. The ERT market is dominated by NAGLAZYME (BioMarin), but the entry of gene therapies and next-generation treatments could transform the competitive landscape. Regulatory incentives for orphan drug development, including market exclusivity and tax benefits, are driving increased investment in rare disease research.

Mucopolysaccharidosis Type VII (Sly Syndrome)
Mucopolysaccharidosis VII (MPS VII), also known as Sly syndrome, is a rare inherited metabolic disorder. MPS VII is caused by mutations in the GUSB gene, which encodes β-glucuronidase. These mutations reduce or eliminate enzyme activity, preventing the breakdown of GAGs. The resulting buildup of GAGs in cells and tissues leads to progressive organ dysfunction and neurological decline. MPS VII is inherited in an autosomal recessive manner, meaning a child must inherit a mutated copy of the gene from both parents to develop the condition.
MPS VII is typically diagnosed in childhood, with symptoms including developmental delays, coarse facial features, organ enlargement, hearing loss, and joint stiffness. The estimated global prevalence of Sly syndrome is about 1 in 250,000 live births, with higher incidence rates in certain regions due to genetic factors.
Enzyme replacement therapy is the primary treatment, involving the administration of synthetic β-glucuronidase to help break down GAGs. However, ERT is limited in addressing neurological symptoms because the enzyme cannot effectively cross the blood-brain barrier (BBB). Research is ongoing to develop therapies that can overcome this challenge, including gene therapy and substrate reduction therapy (SRT), which aim to reduce GAG production or enhance enzyme delivery to the central nervous system.
The MPS VII treatment market is expanding as more companies focus on developing innovative therapies. Leading players include Regenxbio and Ultragenyx Pharmaceutical, which are advancing gene therapy approaches. Other companies are exploring improved ERT and SRT options. Growing awareness of MPS VII, improved diagnostic capabilities, and advancements in genetic treatments are expected to drive market growth in the coming years, increasing the availability of more effective treatment options for patients.
Mucopolysaccharidosis Type IX (Hyaluronidase Deficiency)
Mucopolysaccharidosis IX (MPS IX), also known as hyaluronidase deficiency, is an extremely rare lysosomal storage disorder caused by mutations in the HYAL1 gene, which encodes the enzyme hyaluronidase-1. This enzyme is essential for the degradation of hyaluronan, a glycosaminoglycan (GAG). Deficiency of hyaluronidase-1 leads to the accumulation of hyaluronan in the lysosomes of various tissues, resulting in joint abnormalities, soft tissue masses, and mild facial dysmorphism.
Due to the limited number of documented cases, the exact prevalence of MPS IX is unknown, but it is considered one of the rarest lysosomal storage disorders. Diagnosis is typically confirmed through genetic testing and enzymatic assays measuring hyaluronidase activity. Currently, there is no approved disease-modifying treatment for MPS IX. Management is primarily symptomatic, focusing on improving joint function and addressing soft tissue masses through surgical intervention when necessary. Pain management, physical therapy, and supportive care are commonly employed to enhance patient quality of life.
Given the rarity of MPS IX, drug development has been slow, and there are no specific therapies in late-stage clinical development. However, preclinical research exploring enzyme replacement therapy (ERT) and gene therapy holds promise. Advances in gene editing technologies such as CRISPR/Cas9 and viral vector-based gene delivery could offer long-term solutions by restoring functional HYAL1 expression. Additionally, substrate reduction therapies and chaperone molecules are being investigated to enhance residual enzyme activity and reduce GAG accumulation.
The market for MPS IX is expected to remain highly niche due to the small patient population and the challenges associated with clinical development in ultra-rare diseases. However, the increasing focus on rare diseases and the success of orphan drug programs may incentivize biotech companies to invest in innovative treatment approaches. Regulatory incentives, including orphan drug designation, fast-track approval, and market exclusivity, could drive interest in developing targeted therapies for MPS IX. The successful development of gene therapy or enzyme replacement therapy could unlock significant value in the rare disease segment, attracting interest from both established pharmaceutical companies and emerging biotech firms.
What Lies Ahead in Mucopolysaccharidosis Treatment?
The future of mucopolysaccharidosis treatment holds promise with advancements in gene therapy, ERT, and SRT. Gene therapy is particularly exciting, as it aims to address the root cause of MPS by introducing functional copies of the defective gene into patient cells, enabling the production of functional enzymes.
Clinical trials for gene therapy for mucopolysaccharidosis have shown encouraging early results, with improved enzyme activity, reduced GAG accumulation, and better clinical outcomes. Furthermore, ERT is evolving with next-generation formulations designed to improve blood-brain barrier penetration, addressing the CNS symptoms that current therapies often fail to manage effectively.
Advances in SRT are also expanding options for MPS patients by reducing the accumulation of GAGs through small-molecule inhibitors. Innovative approaches such as stem cell transplantation combined with gene editing and chaperone therapy are showing potential in preclinical and early clinical studies.
Additionally, ongoing research into anti-inflammatory treatments and CNS-targeted delivery systems aims to mitigate neurological decline. Personalized medicine, guided by biomarker-based patient stratification, is expected to further optimize treatment outcomes. Collectively, these advancements suggest that the next decade could bring transformative improvements in both life expectancy and quality of life for individuals with MPS.
Downloads
Article in PDF
Recent Articles
- Rising of Orphan Drug Development
- Mucopolysaccharidosis I (MPS I) (Hurler Syndrome) – a lesser developed window
- The growing size of Sanfilippo syndrome Market: Drivers and Barriers
- Hunter Syndrome Market experiences a positive push as the pharma companies spot the untapped oppo...
- BMS, and Exelixis’s Opdivo + CABOMETYX in First-Line Advanced Renal Cell Carcinoma; AIRSUPRA Now ...