Plasma Proteins Therapeutics: Transforming Treatment in Hematology and Beyond
Oct 23, 2024
Table of Contents
Plasma protein therapeutics are revolutionizing the landscape of modern medicine by harnessing the healing potential of the human body. Derived from donated blood plasma, these life-saving treatments are packed with antibodies, clotting factors, and other essential proteins that help manage a wide array of conditions—from hemophilia and immune deficiencies to autoimmune diseases. By tapping into the body’s natural defense mechanisms, plasma protein therapeutics not only offer targeted relief but also enhance the overall quality of life for countless patients.
As the demand for innovative therapies continues to rise, plasma protein therapeutics stand at the forefront of biopharmaceutical advancements. Their ability to be tailored to individual patient needs makes them a game-changer in personalized medicine.
Downloads
Article in PDF
Recent Articles
- AAV Gene Therapies for Hemophilia B Treatment: The Road to a Cure
- Opportunities and Challenges for Cell and Gene Therapies
- AAV Vectors in Gene Therapy: How Recent Clinical Advances are Unraveling New Potentials?
- New Osteoporosis Drug promises to rebuild Bone
- Biogen buys Nightstar; Pacira acquires Myoscience; Horizon Pharma announces pricing; STAT with Sl...
Understanding Plasma Proteins
Plasma proteins are a complex mixture of proteins found in human blood plasma, which is the liquid component of blood. They perform a variety of essential functions that are crucial for maintaining homeostasis and supporting overall health. Plasma proteins can be broadly classified into three categories:
Albumin
Albumin is the most abundant protein in human plasma, comprising approximately 60% of total plasma protein content. It plays a critical role in maintaining oncotic pressure, which helps regulate blood volume and fluid distribution between blood vessels and tissues. Additionally, albumin functions as a carrier protein, binding to various substances, including fatty acids, hormones, and drugs, facilitating their transport in the bloodstream.
Due to its stabilizing effects on blood volume, albumin is frequently used in clinical settings. It is administered to patients experiencing shock, severe burns, liver disease, or kidney disorders to help maintain blood pressure and volume. Albumin is also used in paracentesis and thoracentesis procedures to manage fluid accumulation in the abdominal or chest cavities.
Immunoglobulins (Ig)
Immunoglobulins, commonly known as antibodies, are essential components of the immune system. They play a crucial role in identifying and neutralizing pathogens, such as bacteria and viruses. There are five main classes of immunoglobulins (IgG, IgA, IgM, IgE, and IgD), each serving distinct functions in the immune response.
Intravenous immunoglobulin (IVIG) therapy is derived from pooled human plasma and is used to treat various conditions, including primary and secondary immunodeficiencies, autoimmune diseases, and inflammatory disorders. IVIG therapy helps to modulate the immune response, providing passive immunity and reducing autoimmune activity. Specific immunoglobulin preparations are also available for the treatment of conditions like hemolytic disease of the newborn and certain viral infections.
Coagulation Factors
Coagulation factors are proteins that play a vital role in the blood clotting process, ensuring proper hemostasis. There are several coagulation factors, each with a specific function in the clotting cascade. Key factors include Factor VIII and Factor IX, which are crucial for blood coagulation and are commonly deficient in hemophilia patients.
Plasma-derived clotting factors are used in the treatment and prevention of bleeding episodes in patients with hemophilia and other clotting disorders. These products are administered to replace the deficient factors, allowing for normal clot formation. Advances in biotechnology have also led to the development of recombinant clotting factors, which offer alternatives to plasma-derived products and reduce the risk of blood-borne infections.
Potential Applications of Plasma Protein Therapeutics
Plasma protein therapeutics have a wide range of applications, significantly impacting the treatment of various medical conditions. Below are key areas where these plasma protein therapeutics are utilized:
Hemophilia Treatment
Hemophilia is a genetic bleeding disorder caused by a deficiency in specific clotting factors, leading to prolonged bleeding and joint damage. Plasma protein therapeutics, particularly clotting factor concentrates derived from human plasma, are essential for managing this condition. These therapies help restore the missing clotting factors in patients, allowing for effective hemostasis during surgical procedures and after traumatic injuries. Patients with hemophilia A, which is caused by a deficiency in factor VIII, and hemophilia B, resulting from a deficiency in factor IX, rely on these therapies for routine prophylaxis and on-demand treatment of bleeding episodes.
In recent years, advancements in biotechnology have led to the development of recombinant clotting factors that provide a safer and more effective alternative to plasma-derived products. These recombinant factors can also be engineered for extended half-lives, allowing patients to experience less frequent dosing and improved quality of life. Furthermore, innovative approaches such as gene therapy are being explored to offer potential curative options for hemophilia, signaling a promising future for patients affected by this condition.
Genetic Disorders
Genetic disorders often result in the absence or dysfunction of specific proteins, leading to various health challenges. Plasma protein therapeutics, such as enzyme replacement therapies (ERT), play a critical role in managing these disorders. For instance, patients with conditions like alpha-1 antitrypsin deficiency can receive infusions of the missing protein to mitigate the risk of lung and liver damage. Similarly, ERTs for lysosomal storage disorders, such as Gaucher disease and Fabry disease, help replenish deficient enzymes, improving symptoms and enhancing patient quality of life.
The use of plasma-derived therapies is complemented by ongoing research into gene therapy and other novel approaches aimed at correcting the underlying genetic defects. Advances in gene editing technologies hold promise for potentially curative treatments, offering hope for patients with genetic disorders who have historically faced limited therapeutic options. By continuing to innovate in this area, the medical community aims to provide more effective and lasting solutions for individuals affected by these challenging conditions.
Neurological Disorders
Plasma protein therapeutics have made significant strides in treating various neurological disorders, particularly through the use of immunoglobulins. Intravenous immunoglobulin (IVIG) therapy is commonly employed to manage autoimmune neurological conditions such as Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy (CIDP). In these cases, IVIG helps modulate the immune system, reducing inflammation and promoting recovery by providing a broad spectrum of antibodies that neutralize harmful autoantibodies targeting the nervous system.
Research continues to explore the potential benefits of plasma protein therapies in other neurological conditions, including multiple sclerosis and neurodegenerative diseases. While the mechanisms are still being elucidated, early studies suggest that plasma-derived therapies may offer neuroprotective effects, supporting nerve regeneration and potentially improving clinical outcomes. As understanding of these conditions evolves, plasma protein therapeutics may play a more prominent role in managing neurological disorders.
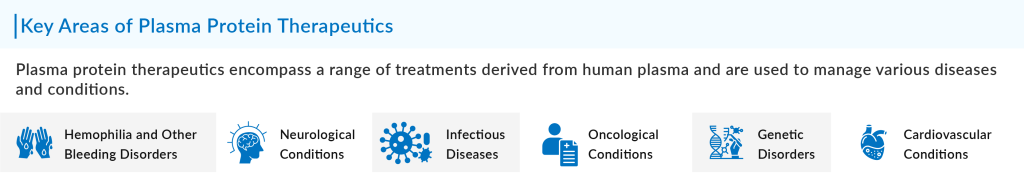
Cardiovascular Conditions
In the realm of cardiovascular medicine, plasma protein therapeutics have emerged as vital components in managing conditions such as acute coronary syndrome and heart failure. Albumin, a key plasma protein, is often used in critical care settings to manage fluid balance, support blood pressure, and enhance tissue perfusion. Its ability to maintain oncotic pressure makes it particularly useful in patients with heart failure or septic shock, where fluid management is crucial to stabilizing hemodynamics and preventing organ failure.
Emerging research is also investigating the potential use of other plasma proteins in cardiovascular therapies. For example, clotting factor concentrates and other derived proteins may be explored for their roles in promoting endothelial repair and reducing inflammation in atherosclerosis. As the understanding of cardiovascular diseases deepens, plasma protein therapeutics could provide additional tools for clinicians in treating and preventing heart-related complications.
Oncology
In oncology, plasma protein therapeutics are increasingly recognized for their role in cancer treatment and management. Immunoglobulin therapies, particularly monoclonal antibodies derived from plasma proteins, have revolutionized cancer care by targeting specific antigens on cancer cells. These therapies enhance the immune response against tumors, leading to improved outcomes for patients with various malignancies, including lymphoma, leukemia, and solid tumors.
Additionally, plasma-derived products such as albumin-based nanoparticles are being developed for drug delivery systems in oncology. These innovative approaches enhance the bioavailability and efficacy of chemotherapeutic agents while minimizing side effects. As research in this field continues to progress, plasma protein therapeutics are likely to play a growing role in personalized cancer treatments, offering new hope to patients battling this challenging group of diseases.
Infectious Diseases
Plasma protein therapeutics are vital in treating infectious diseases, particularly through the use of immunoglobulin preparations. Intravenous immunoglobulin (IVIG) is employed to treat patients with severe infections, immune deficiencies, and autoimmune conditions. By providing a concentrated source of antibodies, IVIG enhances the immune response, helping to neutralize pathogens and control infections. It has proven effective in conditions like severe sepsis, where rapid intervention is critical to patient survival.
In the context of emerging infectious diseases, plasma-derived therapies have gained renewed attention. Convalescent plasma therapy, which involves transfusing plasma from recovered COVID-19 patients to those currently infected, has been explored as a potential treatment strategy. This approach leverages the presence of neutralizing antibodies in the donor plasma to aid the recipient’s immune response. Ongoing research will continue to assess the efficacy and safety of such therapies, highlighting the importance of plasma protein therapeutics in infectious disease management.
Plasma Protein Therapeutics: Emerging Market Trends and Key Companies
Plasma protein therapeutics are gaining increased attention in the healthcare sector due to their ability to treat a wide array of diseases, including autoimmune disorders, immune deficiencies, hemophilia, and neurological conditions.
With advances in technology, plasma-derived therapies are being enhanced, allowing for more targeted treatments. As per DelveInsight analysis, the plasma protein therapeutics market was valued at USD 25 billion in 2023, growing at a CAGR of 6.65% during the forecast period from 2024 to 2030.
This growth is mainly due to several emerging trends in the market. One of the most significant trends in the industry is the rising demand for immunoglobulin (IG) therapies, driven by increasing awareness of primary immunodeficiency (PI) and autoimmune diseases.
Additionally, the aging population worldwide is contributing to a higher demand for plasma-based products to treat age-related chronic conditions. As innovation continues to progress, companies are exploring new plasma protein therapies, with a focus on improving production efficiency and expanding their therapeutic applications.
Another emerging trend in the plasma protein therapeutics market is the focus on sustainable plasma supply. Plasma collection is a time-consuming process that heavily relies on donors, and supply chain disruptions can affect treatment availability. As a result, companies are investing in strategies to increase plasma donations and improve collection efficiency.
Furthermore, ongoing research into recombinant technologies aims to reduce dependency on human plasma by creating alternative protein therapies. Additionally, several key players dominate the plasma protein therapeutics market, leveraging their expertise in research, manufacturing, and distribution to maintain competitive advantages. CSL Behring, a global leader, focuses on developing and distributing a wide range of plasma-derived therapies, including immunoglobulins, coagulation factors, and albumin.
Grifols is another major player, known for its robust plasma collection network and pioneering plasma fractionation technologies. Meanwhile, companies like Takeda Pharmaceuticals, following its acquisition of Shire, have expanded their footprint in rare disease therapies, including plasma-derived treatments.

Some of the other companies currently active in the plasma protein therapeutics segment include Octapharma AG, Biotest AG, Bayer AG, Baxter, Bio Products Laboratory Ltd, Kedrion S.p.A, China Biologic Products Holdings, Inc., and others.
These companies, along with emerging biotech firms, are driving advancements in the market by focusing on improving the therapeutic profile of plasma proteins, enhancing patient access, and expanding into new therapeutic areas such as neurology and immunology.
Plasma Protein Therapeutics: Challenges and Future Directions
Despite the potential applications of plasma protein therapeutics in treating various diseases, the market faces several key challenges. One of the most pressing issues is the supply-demand imbalance. Plasma collection is a labor-intensive and costly process, and with the increasing global demand for these therapies, there is a risk of shortages.
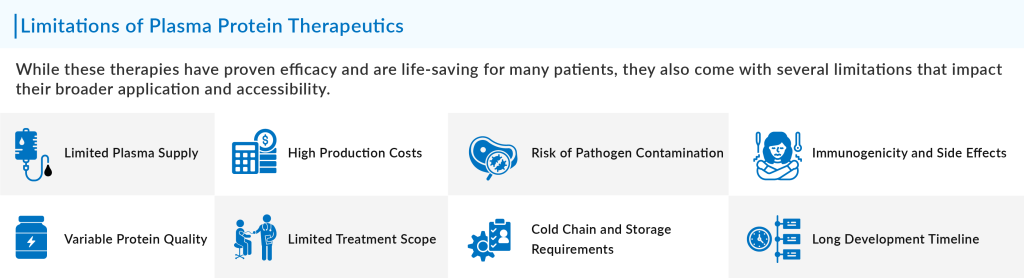
Additionally, there are concerns related to the safety and quality of plasma donations, including the risk of viral contamination, despite stringent screening and purification processes. Regulatory challenges further complicate the development and distribution of new plasma-derived therapies, as they must meet rigorous safety and efficacy standards in various regions, leading to delays and increased costs.
To address these challenges, several innovative strategies are being explored. The future of plasma protein therapeutics may see advancements in recombinant technologies and gene therapies that aim to reduce the reliance on plasma donations. Recombinant proteins, which can be produced in cell cultures, offer the potential for unlimited supply and lower contamination risks. Gene therapies could provide a more permanent solution by targeting the underlying genetic causes of diseases treated by plasma-derived therapies.
Additionally, innovations in purification methods, such as using more efficient chromatographic techniques, may enhance the scalability and reduce the costs of plasma-based products. There is also growing interest in developing synthetic plasma proteins through bioengineering, which could further revolutionize the field by offering more consistent and safer alternatives to traditional plasma-derived therapeutics.
Downloads
Article in PDF
Recent Articles
- Nucleic Acids and Gene Therapies in Neuromuscular Disorders: Next-Generation Therapeutic Strategies
- The Future is Here: BioMarin’s Roctavian First Hemophilia A Gene Therapy Paving the Way for a Cure
- Gene Therapies as a Game-Changer in Ophthalmology: Eyeing the Future
- Gene Therapy Market
- Hemophilia A- Market Scenario