TECELRA Approval for Synovial Sarcoma Treatment – A Ray of Hope
Aug 12, 2024
Adaptimmune Therapeutics and patients waiting for synovial sarcoma treatment witnessed a historic moment at the start of this month. After over ten years without new synovial sarcoma treatments, a groundbreaking, first-in-class cell therapy, TECELRA (afamitresgene autoleucel) has been approved by the FDA.
This also marks the first approval for the 16-year-old company Adaptimmune Therapeutics, which has gained and lost partnerships with major pharmaceutical companies such as GSK, Astellas, and most recently Roche. These companies were initially interested in Adaptimmune’s distinctive engineered T-cell receptor (TCR) platform, which allows for the modification of T-cells to target and eliminate various types of solid tumor cancers. The one-time therapy has a listed price of $727,000.
Adaptimmune Therapeutics’ TECELRA is approved for use in adults with advanced MAGE-A4+ synovial sarcoma who have specific human leukocyte antigen (HLA) types and have previously undergone chemotherapy. These patients are required to have their genetic HLA types and MAGE-4A expression tested through a companion diagnostic screening.
Downloads
Article in PDF
Synovial sarcoma is a relatively rare cancer, classified as a soft tissue sarcoma with unclear differentiation. It constitutes 5–10% of all STS cases. About 70% of those with synovial sarcoma show the MAGE-A4 antigen. The disease predominantly impacts younger people, with about a third of cases occurring in individuals under 30. In 2023, the US had the highest number of synovial sarcoma cases among the 7MM, with ~650 cases, and this number is projected to rise in the coming years, as per DelveInsight.
The approval of TECELRA for synovial sarcoma treatment was based on the results from the SPEARHEAD-1 (Cohort 1) trial, which involved 44 patients. The primary measure of effectiveness was the overall response rate (ORR) as determined by an independent review, which was further supported by the duration of the response.
TECELRA synovial sarcoma treatment achieved an ORR of 43% with a complete response rate of 4.5%. The median duration of response was 6 months (95% CI: 4.6, not reached). Among those who responded to the treatment, 39% had a response lasting 12 months or more. The key findings from the SPEARHEAD-1 trial were published earlier this year in The Lancet.
TECELRA may lead to severe side effects such as cytokine release syndrome (CRS), immune effector cell–associated neurotoxicity syndrome (ICANS), prolonged and severe drops in blood cell counts, infections, secondary cancers, and hypersensitivity reactions. The most frequently occurring adverse effects (with an incidence of 20% or more) include CRS, nausea, vomiting, fatigue, infections, fever, constipation, shortness of breath, abdominal pain, non-cardiac chest pain, decreased appetite, rapid heartbeat, back pain, low blood pressure, diarrhea, swelling, and reductions in white blood cells, red blood cells, and platelets.
Before starting TECELRA treatment, it is necessary to conduct biomarker tests for human leukocyte antigens (HLA) type and melanoma-associated antigen A4 (MAGE-A4) tumor expression. Adaptimmune has collaborated with Agilent Technologies to develop, manufacture, and supply a companion diagnostic for the MAGE-A4 biomarker, known as MAGE-A4 IHC 1F9 pharmDx, which has just received approval from the U.S. FDA and is now available. Additionally, the company has teamed up with Thermo Fisher Scientific to expand the labeling of Thermo Fisher’s SeCoreTM CDx HLA-A Locus Sequencing System to include TECELRA, facilitating the identification of HLA-A02:01, A02:02, A02:03, and A02:06-positive patients with synovial sarcoma.
Adaptimmune went public in 2015 but faced significant challenges in April when Genentech, in a cost-cutting move, ended a $3 billion partnership aimed at developing two allogeneic T-cell therapies targeting up to five different indications.
However, just seven weeks later, Galapagos stepped in with a $665 million agreement for the rights to uza-cel, a MAGE-4A TCR T-cell therapy that Adaptimmune is testing in phase II trials for ovarian cancer. The Belgian biotech plans to explore uza-cel for head and neck cancer and potentially other solid tumors. The deal with Galapagos, which includes an initial $100 million payment, will support Adaptimmune’s launch of TECELRA.
With this TECELRA approval, Adaptimmune is set to greatly influence the synovial sarcoma treatment space. Healthcare professionals can start evaluating patients, Adaptimmune’s systems are prepared to process TECELRA orders, and the AdaptimmuneAssist program is in place to provide a smooth and tailored experience throughout the treatment process. Adaptimmune aims to establish between six and ten authorized treatment centers (ATCs) this year and to integrate around 30 ATCs within the first two years. These centers are prominent in synovial sarcoma research and treatment.
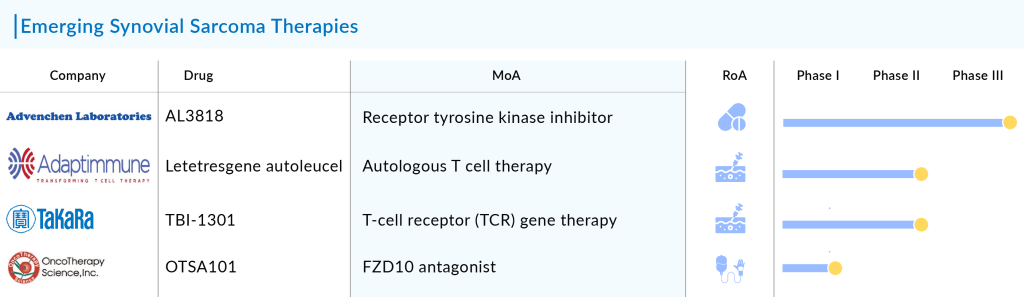
Adaptimmune is also working with its other synovial sarcoma treatment candidate Letetresgene autoleucel. Letetresgene autoleucel (Lete-cel) is a specialized TCR T-cell therapy designed to target the NY-ESO-1 antigen found in solid tumors. Currently under investigation in the IGNYTE-ESO trial (NCT03967223), lete-cel is being tested for its effectiveness in synovial sarcoma treatment and myxoid/round cell liposarcoma (MRCLS) in patients who have previously received anthracycline treatment. The trials for lete-cel are now sponsored by Adaptimmune, following a transition from GSK.
Although the IGNYTE-ESO trial is ongoing, it is not accepting new participants. The interim analysis data was presented at CTOS in 2023, and sub-study 1 of the trial is exploring the use of lete-cel as a first-line treatment for newly diagnosed patients with metastatic or unresectable synovial sarcoma or MRCLS. The company aims to commercially launch lete-cel in the US by 2026, marking the introduction of a second synovial sarcoma treatment option and expanding available therapies for these cancers.
Apart from Adaptimmune, Takara Bio is also evaluating T-cell receptor (TCR) gene therapy TBI-1301. The drug is currently in Phase I/II synovial sarcoma clinical trials. The anticipated launch will give an edge in the synovial sarcoma treatment market.
In addition to TCR T-cell therapies, several other emerging drug classes and novel therapies are being investigated for synovial sarcoma treatment. These include FZD10 antagonists that target the FZD10 receptor, which is involved in the Wnt signaling pathway—a key player in cancer development, and tyrosine kinase inhibitors that target vascular endothelial growth factor receptors (VEGFR), aiming to disrupt tumor blood supply.
Although promising, the full potential of FZD10 antagonists in synovial sarcoma treatment remains under investigation, with further studies needed to confirm their effectiveness and integrate them into standard treatment protocols. OncoTherapy Science’s OTSA101 is an anti-FZD10 antibody and has been developed as a novel cancer therapy for synovial sarcoma treatment. The drug is currently in Phase I synovial sarcoma clinical trials.
In the tyrosine kinase inhibitors segment, Advenchen Laboratories is working on its lead asset AL3818. Advenchen Laboratories’ AL3818 is being evaluated for the treatment of alveolar soft part sarcoma, leiomyosarcoma, and synovial sarcoma in a global Phase III synovial cancer clinical trial. The both FDA and EMA have granted AL3818 an orphan drug designation for the potential treatment of soft tissue sarcomas.
Several other innovative approaches are also being explored to enhance synovial sarcoma treatment options. With the launch of these emerging synovial sarcoma therapies, the landscape of the synovial sarcoma treatment market is expected to change in the coming years.
Additionally, a significant amount of research and developmental activities over the past several years have led to the gradual emergence of more effective and less toxic treatment modalities in synovial sarcoma patients. As a result, patients will have access to synovial sarcoma treatments in the future that offer better outcomes and reduced side effects, ultimately enhancing their quality of life and providing new hope for long-term remission.
Downloads
Article in PDF